Pharmacist prescribers Linda Bryant and Leanne Te Karu discuss positive polypharmacy for heart failure. Current evidence shows the intensive implementation of four medications offers the greatest benefit to most patients with heart failure, with significant reductions in cardiovascular mortality, heart failure hospitalisations and all-cause mortality
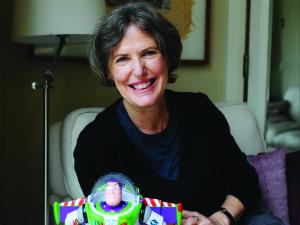
Never look back: Waimate GP gives her all for community
Never look back: Waimate GP gives her all for community

From solo GP duties to community care and flexible working practices, Sarah Creegan’s life is about balancing the challenges of rural medicine with love for her patients and her town. Zahra Shahtahmasebi reports
When Sarah Creegan’s adult children asked her why she moved their family nearly 1500km from Great Barrier Island to Waimate, she shrugged and said, “It seemed like a good idea at the time.”
It has been about 17 years since that move, which led to Dr Creegan, a specialist GP, taking over Waimate Medical Centre. The small Canterbury town is an excellent place to live, she says.
“I’ve had the huge privilege of living in some really lovely parts of New Zealand and the place that I’m in now very much is the home that I love.”
- Location: 84 Queen Street, Waimate 7924.
- PHO: Primary and Community Health Aotearoa.
- Staff: One GP, one remote doctor, six nurses, one health coach, one health improvement practitioner, four receptionists, one practice manager, one extended care paramedic.
- Owner: Specialist GP Sarah Creegan.
- Enrolled patients: Just over 2600.
- Funding: Capitation, rural, acute care demand.
Dr Creegan and her husband bought Waimate Medical Centre from the local council in 2007. Although the practice was purpose-built in 1961, it was outdated in many ways, she says.
Under her leadership, Waimate Medical Centre became Cornerstone-accredited. In December 2018, the team moved into a new building with the help of local businessperson Gary Rooney.
“It’s a real point of pride for me to work in that space…it’s nothing architecturally clever particularly, but it’s functional and a really pleasant space to work in,” says Dr Creegan.
The practice has a large staff room, which seemed an extravagant addition at the time as it could have allowed for another couple of consultation rooms, she adds.
“But it’s proved worth it because the key struggle for all of us now is recruiting and retaining staff, and having that big space makes it materially obvious how much we value our staff.”
Waimate Medical Centre is colocated with the local pharmacy on 84 Queen Street and is open Monday to Friday, 8.30am to 5.30pm.
After-hours care used to be provided by Dr Creegan, who would remain on call after the practice closed, but she says Te Whatu Ora recently released Waimate Medical Centre from this commitment.
After hours is now managed through the Ka Ora Telecare, which provides video and phone consultations. Any patients requiring secondary care travel north to Timaru Hospital or south to Oamaru Hospital.
While she felt guilty about stopping her after-hours service, it was necessary to maintain and sustain her practice, especially as a primarily solo GP.
“I suddenly thought, ‘When was I last not on call all the time? I’ve been doing rural medicine, and all the on-call associated with it since 2003,” says Dr Creegan.
The money she has saved from no longer providing after hours has fed back into the practice and allowed her to give her nursing team a pay increase.
So far, the community has received the switch to Ka Ora well.
Most of her peers and colleagues are part time or retired, and she constantly hears statistics about the alarming number of GPs retiring in the next five to 10 years.
But there are no conversations about how to retain them, she adds.
“How do we retain people like me? Well, you retain me by actually giving me, for the first time ever, Christmas and New Year off.”
Don’t get her wrong; she still has her Primary Response in Medical Emergency (PRIME) commitments as well as the local resthome and palliative care patients – but removing after hours has helped in achieving an improved work–life balance.
The Waimate Medical Centre is grateful to be a member of Primary Community and Health Aotearoa and receives capitation, rural funding and, most recently, acute care demand funding, Dr Creegan says.
She is also grateful for the support from Te Whatu Ora, whose national model she believes will help to iron out the inequities experienced in rural health.
Waimate is home to a downto-earth population, many of whom have spent decades working in their local community, says Dr Creegan.
The practice has just over 2600 enrolled patients, with a high percentage of Community Services Card holders and people over 65. There is a small number of Māori – about 10 per cent – and increasing numbers of Nepalese and Filipino people, who often move to Waimate to work in the dairy and rural industries.
A lot of the practice’s energy goes into its older population, who present with ischaemic heart disease, chronic obstructive pulmonary disease, cancer and dementia, says Dr Creegan.
Then there are the freezing workers with shoulders and joints that are not fit for purpose, the retired shearers who smoked every day after work and have a multitude of health problems, including lung cancer and COPD, or the teenagers and young adults who are vaping, she adds.
All are important to Dr Creegan, who recently told her medical students that she loves her patients. “And they just looked at me – and I said to them, ‘You’re allowed to love your patients.’”
Waimate Medical Centre prides itself on providing same-day appointments for patients who need them. Since COVID-19, the practice has employed a red and green stream to separate unwell patients from the others. Nurses work at the top of their scope to triage and assess those who need to be seen urgently, and the GP must be flexible and move from patient to patient as needed.

The practice books are closed, but exceptions are made case-by-case for families with young children to ensure they get their necessary immunisations, says Dr Creegan. Otherwise, she controls the patient population carefully to maintain the sanity of herself and her staff.
“Which is a contradiction, really, in terms of what you are trying to do for your community. It’s pretty hardcore when you know someone’s high needs,” she says.
“I have got a population of people who really, really need good general practice because, without it, they’re failing.”
While primary care is challenging, she cannot speak highly enough of Waimate and its community. New additions, including a 60km walking and cycling track and the regeneration of bird life thanks to a predator-free fence, are bringing positive change to the township.
“So, the little understated, perhaps slightly scruffy look of Waimate is gradually changing,” says Dr Creegan.
While there were several reasons for Dr Creegan to take the leap and move her young family from their home on Great Barrier Island, she can think of one word to sum up her decision 17-odd years ago: “It’s freedom. We’ve got freedom on the property to charge around. We have a pretty fun life, really.”
Dr Creegan describes the team as cohesive, connected and compassionate despite the intense and complex workload they face every day at the practice.
The acute care demand funding rolled out to the practice on 1 August, was a long-awaited recognition and a spotlight on all that goes on at the centre, she adds.
That same day, a patient with a heart problem and dementia living on the edge of town experienced complications and needed urgent attention. Simultaneously, a patient at the resthome vomited and lost consciousness while another patient walked into the practice with a nosebleed that would not stop. “On the first day of the funding, I was laughing to myself because I thought, ‘They’re never going to believe that this is what happens’,” says Dr Creegan.
With acute demand funding, the practice could treat the patients locally without calling an ambulance and sending them to Timaru Hospital.
Dr Creegan’s team currently consists of herself as the solo GP, six nurses, four receptionists, a practice manager, a health coach and health improvement practitioner, and an extended care paramedic through a Te Whatu Ora pilot project.
Dr Creegan’s former classmate, friend and doctor Jim McLeod works for Waimate Medical Centre remotely from Northland, completing scripts, performing phone consults and inbox analysis. Dr McLeod has worked at the practice in person so is familiar with the staff, centre and the town.
The practice also benefits from medical student attachments, locum GPs and regular visits from a midwife and the recently retired head of Plunket, Raelene Todd, who is also a member of Dr Creegan’s book group.
“She’s an absolute delight...such an incredibly valuable workforce member. She’s vaccinating babies and doing health checks on children. So, it’s really lovely for our patients.”
Staff recruitment is as challenging as ever, and with so much of general practice reliant on the generosity of its people, Dr Creegan finds she needs to be creative to sustain her practice and her succession plan.
“I still love medicine, but I don’t love it when it’s just me – it’s really intense, and doing 10 to 12-hour days is so unappealing. It truly sickens me that safe and effective delivery of general practice care relies so heavily on goodwill and good luck.”
As a result, Waimate Medical Centre has become more flexible, allowing staff to work family-friendly hours or from home if their kids are sick.
The move to the cloud-based practice management system, Medtech Evolution, in May 2020 was a tremendous help, streamlining systems and making remote work possible.
Accommodation is a challenge for potential staff members looking to relocate to Waimate, so, last year Dr Creegan renovated a local home with the help of interior designer Deborah Still to make the move more appealing.
She has also recently welcomed new team member Echo, a mini-Schnauzer puppy, who she plans to train up to host patients in the waiting room.
Most of all, Dr Creegan is proud of what her team continues to deliver: thorough, respectful and effective general practice care. “As a team, we do incredibly well despite the challenges that continue to frustrate, erode and undermine everything we rely on to do our jobs.”
Zahra Shahtahmasebi is an Auckland journalist
We're publishing this article as a FREE READ so it is FREE to read and EASY to share more widely. Please support us and our journalism – subscribe here
One of the benefits of subscribing is you will also be able to share your thoughts about what you read with others in our Comment Stream. You can also take notes on what you read with Capture