Respiratory physician Lutz Beckert considers chronic obstructive pulmonary disease management, including the prevention of COPD, the importance of smoking cessation and pulmonary rehabilitation, and the lifesaving potential of addressing treatable traits. He also discusses the logic of inhaler therapy, moving from single therapy to dual and triple therapy when indicated, as well as other aspects of management
Patients to be hit hard after too-little, too-late 4% offer
Patients to be hit hard after too-little, too-late 4% offer

Expecting the public to bear the brunt of the Government’s ‘absolutely inadequate’ and ‘demoralising’ 4 per cent capitation offer through patient fee hikes is exasperating general practice leaders. Fiona Cassie summarises the feedback received by New Zealand Doctor Rata Aotearoa as the ‘underwhelming’ offer goes out to consultation
Budget-pinched Te Whatu Ora telling practices they can increase patient fees, on average, by 7.76 per cent to make up for the capitation funding shortfall has drawn a sharp response from primary care leaders.
Hauora Taiwhenua Rural Health Network chief executive Grant Davidson describes the “underwhelming” offer as a “cost-shifting exercise to the general public who are already in a cost-of-living crisis”.
General Practice Owners Association deputy chair Stephanie Taylor agrees, saying the “Government basically [is] going to shift the cost of providing that GP care onto the patients, which none of us supports”.
The “disproportionate” proposed increase in patient fees is also noted in a media release by General Practice Leaders Forum chair and RNZCGP president Samantha Murton, who says the “disappointing” offer could see patients picking up the shortfall in funding.
Likewise, General Practice NZ chair and specialist GP Bryan Betty says the expectation that patient fee increases will compensate for the “absolutely inadequate” funding will mean patients “bear the brunt again”.
For many, Nelson specialist GP Graham Loveridge says that any tax benefit under Budget 2024 could be “neutralised” by potentially higher GP fees and prescription charges.
General practice leaders also voiced their frustration at the Coalition Government’s lack of action on its preelection commitments to implement the 2022 Sapere report.
Dr Davidson recalls all coalition partners before the election saying they would work to resolve chronic underfunding highlighted by the report. “But [the offer] is not even keeping pace with inflation.”
Māpua specialist GP, Andre Bonny, agrees, saying the proposed increase is “nowhere near the amount needed” and points to the ACT Party’s preelection promise of a 13 per cent capitation increase.
GenPro chief executive Mark Liddle echoes Dr Bonny’s reference to ACT’s promise, adding that ACT and National both campaigned on the 2022 Sapere report and the need to address underfunding: “But they haven’t delivered.” The Sapere report indicated that most practices needed a median capitation rise of 10 to 20 per cent and much more for very-high-needs practices.
ACT leader and associate health minister David Seymour, in an email, says the country’s “dire fiscal situation” meant that not all policies campaigned on were included in the Coalition Government’s first Budget.
Primary care leaders also expressed exasperation at the capitation increase’s failure to recognise the sector was in crisis due to long-standing underfunding and workforce pressures.
Dr Taylor, a specialist GP, says GenPro warns of the risk of more practice closures after a capitation offer that “definitely falls short” of stabilising the already financially struggling sector.
“In an ideal world, we would have seen a double-figure investment just to stabilise general practice,” Dr Taylor says. Failing to invest in chronically underfunded practices will force them to increase fees or decrease the services they provide just to remain viable.
Dr Betty says: “We know that a lot of practices are becoming marginal in terms of their sustainability, and this just adds to the pressure…”
Health minister Shane Reti has indicated he is most interested in the 2025/26 Budget, Dr Betty says. “However, that’s another year’s delay in sorting out the underlying funding problems.”
RNZCGP medical director Luke Bradford says the 4 per cent offer is “patently below” what’s needed to rectify chronic underfunding. Dr Bradford argues that relying on fee increases to cover underfunding risks limiting patient access to care and pressures practices to bear the cost of discounting care or carrying patient debt.
Mr Liddle agrees, saying he spoke to a GenPro practice, which gets half its income from capitation. Its patients can’t afford a fee increase so that effectively halves the increase the practice could receive in 2024/25 from 4 per cent to just 2 per cent, he says.
Very Low Cost Access general practice leaders also rejected the suggestion from Te Whatu Ora that struggling high-needs practices can boost income by charging higher fees to non-Community Services Card holders.
Lloyd McCann, chief executive of Tāmaki Health, which owns many VLCA practices, says the suggestion was unworkable and “purely theoretical” as there was “no way we can put our fees up...Our patients, a lot can’t afford another $10; people are already making decisions between seeing the doctor or putting food on the table.”
Dr McCann says the proposed capitation increase is “incredibly demoralising”, and the sector needs a public outcry like that which resulted in the Government's U-turn on funding new cancer drugs.
“Especially as, while such drugs are important, we know everything starts and ends in primary care, and if we don’t make a decision to invest in this sector, you can have the extra stuff you like, but you will still have inequitable health outcomes.”
National Hauora Coalition chief executive Rachel Brown says, by email, that charging non-CSC holders more would impose a significant financial burden on whānau already feeling the pinch. “This decision will only perpetuate Māori health inequities.”
The coalition and other Māori PHOs are calling for an in-person hui to find more effective solutions, she says. “Our focus remains advocating for a re-prioritisation of funding, aligning with our overarching commitment to delivering equitable outcomes for Māori and other high-needs populations who deserve better healthcare.”
Procare chief executive Bindi Norwell says the lacklustre offer leaves practices with little option than to raise fees, making a GP appointment unaffordable for some patients and pushing more to queue at hospital emergency departments.
“The entire healthcare system is already in crisis, and this inadequate capitation offer adds more fuel to the fire,” Ms Norwell says in an email.
WellSouth Primary Health Network chief executive Andrew Swanson-Dobbs, also by email, says the offer “signalled a lack of commitment” by the board of Te Whatu Ora to address the sector’s deep-seated underfunding.
“This will not address our southern challenges: our large rural population, our workforce pressures and, like other regions, our continued inequitable health outcomes.”
Total package
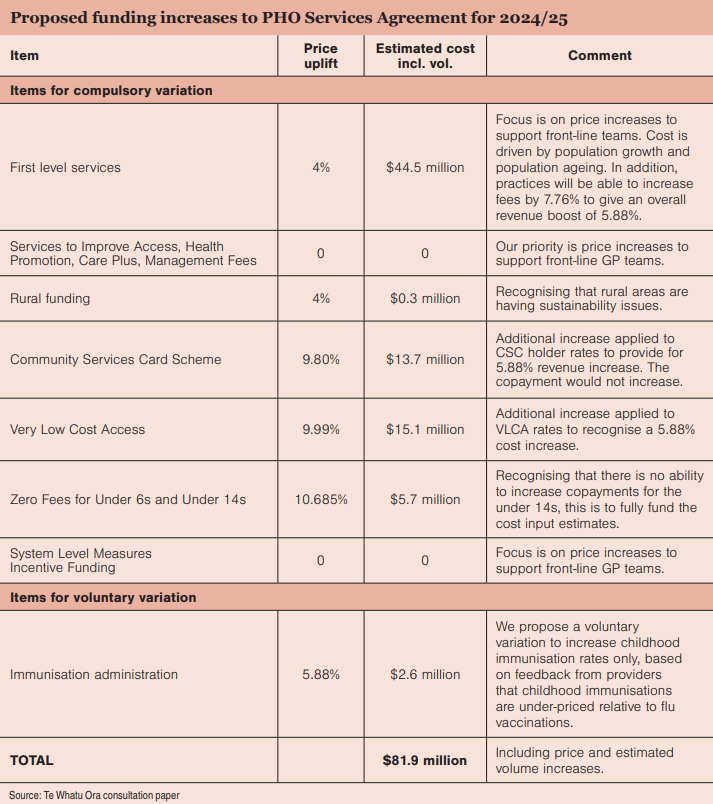
- $81.9 million is the estimated cost of the proposed Te Whatu Ora package to cover funding increases and patient volume increases under the PHO Services Agreement in 2024/25.
Cost pressure
- 5.88 per cent is the costpressure figure for general practices for 2024/25, calculated using the Annual Statement of Reasonable Fees Increase formula.
Capitation offer
- 4 per cent is the funding offer for first-level services capitation, which makes up about 80 per cent of capitation funding (a $44.5 million increase).
Patient fee increase
- 7.76 per cent is the average patient fee increase proposed by Te Whatu Ora so practices can make up the funding gap between the agency’s 4 per cent capitation offer and the 5.88 per cent cost pressure figure (ie, for practices with a 50/50 split in income between capitation and fees).
- 8.7 per cent to 13.39 per cent is the patient fee increase practices that receive between 60 to 80 per cent of their income from capitation (60/40 to 80/20 splits) can charge.
Capped and zero-fee funding offers
- 9.8 per cent to 10.68 per cent are the higher offers being made for the Very Low Cost Access, Community Services Card and Zero Fees for Under-14s funding streams to deliver “an effective increase of 5.88 per cent” (combined value of $34.5 million).
- $19.50 is proposed to remain the maximum CSC patient fee/ copayment, but Te Whatu Ora is “open” to VLCA practices that are “struggling financially” to increase patient fees to non-CSC patients.
Flexible funding stream offer
- 0 per cent is the increase offered to a range of PHO-administered funding, including Services to Improve Access, Health Promotion, Care Plus, PHO management fees and System Level Measures incentive funding.
Carried-over pay parity and equity funding
- $31 million in nurse pay-parity funding and $22 million in equity-adjuster funding – both delivered last year outside PHO Services Agreement – are also to be extended.
High cost rises and low government funding could see patient fee increases of up to 13.39 per cent allowed at some practices – the highest ever allowed under capitation funding.
However, in an emailed statement, Te Whatu Ora Living Well director Martin Hefford says that while the agency sets the maximum fee increase, general practices decide their fee increases, and the “actual fees vary considerably”.
Consultant Sapere, which has calculated the Annual Statement of Reasonable Fee Increases for nearly 20 years, says this year’s maximum fee increases “are the highest they have ever been”.
“This reflects the strong rises in input costs and the lower relative government funding contribution for this year,” Sapere says in its 2024/25 ASRFI report to Te Whatu Ora. The maximum fee increases range from 7.76 per cent for practices that receive 50 per cent of their income from capitation to 13.39 per cent for practices that rely on capitation for 80 per cent of their funding.
Te Whatu Ora acknowledges the “significant financial and workforce pressure” on general practice sustainability in its consultation paper to the sector on this year’s funding increase, Mr Hefford says. The increased offer considers the 5.88 per cent cost pressure figure, the need to stay within Budget 2024 appropriations, GP financial sustainability issues and the necessity to preserve primary care access for low-income New Zealanders.
With Very Low Cost Access practices in “many cases struggling financially”, the agency proposes a more significant funding increase to that sector. It is “open” to increasing patient fees for non-Community Services Card holders.
Also under consideration is a higher threshold for fee increases before practices had to apply to the Fees Review Committee, which will recognise the “financial issues” facing practices in general.
Possible relief for practices struggling to meet urgent and after-hours care obligations under the PHO Services Agreement due to “workforce constraints” is another proposal.
“Te Whatu Ora is open to considering the development of a protocol under which we would collaborate to address afterhours issues locally,” the consultation document says.
Primary care leaders refused to endorse an “inadequate” government funding offer that didn’t address “chronic underfunding”, an official communique confirms.
The communique, agreed to by members of the PHO Services Agreement Amendment Protocol, was released by Te Whatu Ora after the agency presented the 4 per cent capitation increase to the sector at the PSAAP forum on 19 June (see full offer details in panels).
PSAAP members “expressed significant concerns” at the offer’s “inadequacy” and the “highly unsatisfactory” compressed PSAAP process, which didn’t allow adequate time for negotiations or consultation.
“The overall feedback was that the financial sustainability of the sector is not advanced by this proposal,” the communique says, and “PHOs and contracted providers were unable to endorse the proposal”. The agency agreed to PSAAP members’ requests for a 20-day consultation period with a decision to be made on 20 July so payments could be made in August and back-dated to 1 July.

![NZ cash, money, notes [Thomas Coker on Unsplash]](/sites/default/files/styles/cropped_image_4_3/public/2024-05/thomas-coker-M8fYycGWuMA-unsplash.jpg?itok=0I2O_NFl)


![Tug of war money [Alashi on iStock]](/sites/default/files/styles/cropped_image_4_3/public/2024-03/Tug%20of%20war%20money%20and%20hand_CR_iStock-808110400_alashi.jpg?itok=zKaJClcm)





![Barbara Fountain, editor of New Zealand Doctor Rata Aotearoa, and Paul Hutchison, GP and senior medical clinician at Tāmaki Health [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/Barbara%20Fountain%2C%20editor%20of%20New%20Zealand%20Doctor%20Rata%20Aotearoa%2C%20and%20Paul%20Hutchison%2C%20GP%20and%20senior%20medical%20clinician%20at%20T%C4%81maki%20Health%20CR%20Simon%20Maude.jpg?itok=-HbQ1EYA)
![Lori Peters, NP and advanced health improvement practitioner at Mahitahi Hauora, and Jasper Nacilla, NP at The Terrace Medical Centre in Wellington [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/2.%20Lori%20Peters%2C%20NP%20and%20advanced%20HIP%20at%20Mahitahi%20Hauora%2C%20and%20Jasper%20Nacilla%2C%20NP%20at%20The%20Terrace%20Medical%20Centre%20in%20Wellington%20CR%20Simon%20Maude.jpg?itok=sUfbsSF1)
![Ministry of Social Development health and disability coordinator Liz Williams, regional health advisors Mary Mojel and Larah Takarangi, and health and disability coordinators Rebecca Staunton and Myint Than Htut [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/3.%20Ministry%20of%20Social%20Development%27s%20Liz%20Williams%2C%20Mary%20Mojel%2C%20Larah%20Takarangi%2C%20Rebecca%20Staunton%20and%20Myint%20Than%20Htut%20CR%20Simon%20Maude.jpg?itok=9ceOujzC)
![Locum GP Helen Fisher, with Te Kuiti Medical Centre NP Bridget Woodney [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/4.%20Locum%20GP%20Helen%20Fisher%2C%20with%20Te%20Kuiti%20Medical%20Centre%20NP%20Bridget%20Woodney%20CR%20Simon%20Maude.jpg?itok=TJeODetm)
![Ruby Faulkner, GPEP2, with David Small, GPEP3 from The Doctors Greenmeadows in Napier [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/5.%20Ruby%20Faulkner%2C%20GPEP2%2C%20with%20David%20Small%2C%20GPEP3%20from%20The%20Doctors%20Greenmeadows%20in%20Napier%20CR%20Simon%20Maude.jpg?itok=B0u4wsIs)
![Rochelle Langton and Libby Thomas, marketing advisors at the Medical Protection Society [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/6.%20Rochelle%20Langton%20and%20Libby%20Thomas%2C%20marketing%20advisors%20at%20the%20Medical%20Protection%20Society%20CR%20Simon%20Maude.jpg?itok=r52_Cf74)
![Specialist GP Lucy Gibberd, medical advisor at MPS, and Zara Bolam, urgent-care specialist at The Nest Health Centre in Inglewood [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/7.%20Specialist%20GP%20Lucy%20Gibberd%2C%20medical%20advisor%20at%20MPS%2C%20and%20Zara%20Bolam%2C%20urgent-care%20specialist%20at%20The%20Nest%20Health%20Centre%20in%20Inglewood%20CR%20Simon%20Maude.jpg?itok=z8eVoBU3)
![Olivia Blackmore and Trudee Sharp, NPs at Gore Health Centre, and Gaylene Hastie, NP at Queenstown Medical Centre [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/8.%20Olivia%20Blackmore%20and%20Trudee%20Sharp%2C%20NPs%20at%20Gore%20Health%20Centre%2C%20and%20Gaylene%20Hastie%2C%20NP%20at%20Queenstown%20Medical%20Centre%20CR%20Simon%20Maude.jpg?itok=Z6u9d0XH)
![Mary Toloa, specialist GP at Porirua and Union Community Health Service in Wellington, Mara Coler, clinical pharmacist at Tū Ora Compass Health, and Bhavna Mistry, specialist GP at Porirua and Union Community Health Service [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/9.%20Mary%20Toloa%2C%20Porirua%20and%20Union%20Community%20Health%20Service%20in%20Wellington%2C%20Mara%20Coler%2C%20T%C5%AB%20Ora%20Compass%20Health%2C%20and%20Bhavna%20Mistry%2C%20PUCHS%20CR%20Simon%20Maude.jpg?itok=kpChr0cc)