Respiratory physician Lutz Beckert considers chronic obstructive pulmonary disease management, including the prevention of COPD, the importance of smoking cessation and pulmonary rehabilitation, and the lifesaving potential of addressing treatable traits. He also discusses the logic of inhaler therapy, moving from single therapy to dual and triple therapy when indicated, as well as other aspects of management
Hokianga paramedic wears three hats: Thinking outside the square amid northern doctor shortage
Hokianga paramedic wears three hats: Thinking outside the square amid northern doctor shortage

Here at New Zealand Doctor Rata Aotearoa we are on our summer break! While we're gone, check out Summer Hiatus: Stories we think deserve to be read again! This article was first published on 23 November 2022.
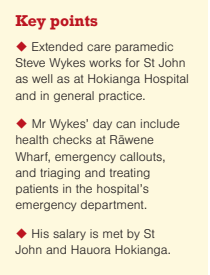
Chosen by Natasha Jojoa Burling: Extended care paramedic Steve Wykes has carved out a niche for himself in the Hokianga and now fulfils three different roles and helps with the GP shortage.
One man who disembarked the ferry with chest pains turned out to be having a heart attack
A St John paramedic whose Northland station was threatened with closure has reinvented himself and is helping fill the doctor shortage by taking on three roles.
A couple of years ago, extended care paramedic Steve Wykes was bored working for St John in Rāwene, on the Hokianga Harbour, because there were so few call-outs. The service was also considering closing the station.
Mr Wykes approached Hokianga Hospital and volunteered to help with anything, including cleaning, just to keep himself busy.
St John and the hospital did a trial to see how it would work, then agreed to each pay half of his salary. He lives 30 minutes to the southeast in Waimamaku and works Monday to Friday 8am to 4.30pm but finishes at 5.30pm most days.
Mr Wykes does triage and treatment at the emergency department and ambulance work and general practice work in the community.
At the hospital, he may be inserting catheters, suturing, and lancing boils and wounds. For anything “above his pay grade”, the patient is sent to the doctor. If there is an emergency, he deals with that until a doctor turns up.
St John pages him when a job comes in: “The only downside is, if the pager goes off, I have to drop everything and run,” he says.
In his ambulance, Mr Wykes covers a “huge area”, travelling as far north as Broadwood, to the other side of the Waipoua Forest, and as far east as Taheke.
As well as emergency call-outs, he does health checks on people waiting for the ferry at Rāwene Wharf.
He parks outside Four Square and does blood pressure readings, blood sugar levels and electrocardiograms in the back of the ambulance. Underlying problems like prediabetes or pre-hypertension are picked up in people who have not seen a doctor for a while.
One person came with a headache: “Your blood pressure’s 230, no wonder,” he said.
And one man who disembarked the ferry with chest pains turned out to be having a heart attack.
Mr Wykes informs most people of their results at the time. If there are concerns, he books them in for a GP appointment, then puts his notes into their files for the doctor to review.
If they have major ailments such as extreme hypertension with symptoms or chest pain, he takes them directly to the hospital. Most of the time he continues treating them there, which includes bloods, ECGs, and medications if necessary. He then passes them over to the doctor.
Since 29 August, Hokianga Hospital has had no doctor from 5pm to 8am. Via email, Hauora Hokianga chief executive Margareth Broodkoorn says the after-hours service has not been stood up for November: “We still continue with medical staff shortages and unable to fulfil a medical after-hours roster.”
The urgent-care clinic at the hospital remains open between 8am and 5pm. Maternity services, aged care long-stay and residential care services also continue, along with Whānau Ora, mental health, social services and home help.
Ms Broodkoorn says there has been an extended care paramedic at Hokianga Health for the past few years as a successful pilot: “The [paramedic] works alongside our doctors and nurses in the urgent-care clinic Monday to Friday. We are in the process of formalising this with St John.”
Mr Wykes says he helps fill in the gaps created by the doctor shortage. When someone phones or is contacted by the hospital and cannot or doesn’t want to come in, or cannot get a GP appointment, he goes out to treat them as a general practice patient. He follows up a few days later and, if they need to be in hospital, he brings them in.
He follows up after-hours patients and can visit them in their homes if needed.
“People only turn up if they are really crook,” he says. One woman who had been having a heart attack for three days was brought in by a neighbour. It showed up in her blood work, so she was taken to Whangārei Hospital.
He says other paramedics could have several roles like his. St John is losing a lot of people to private practice and is running short of qualified staff. He says in a clinic, paramedics are paid “really good money” and there are “no hassles”. The combination of different jobs works for him: “It is interesting work because every day is different,” he says.







![Barbara Fountain, editor of New Zealand Doctor Rata Aotearoa, and Paul Hutchison, GP and senior medical clinician at Tāmaki Health [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/Barbara%20Fountain%2C%20editor%20of%20New%20Zealand%20Doctor%20Rata%20Aotearoa%2C%20and%20Paul%20Hutchison%2C%20GP%20and%20senior%20medical%20clinician%20at%20T%C4%81maki%20Health%20CR%20Simon%20Maude.jpg?itok=-HbQ1EYA)
![Lori Peters, NP and advanced health improvement practitioner at Mahitahi Hauora, and Jasper Nacilla, NP at The Terrace Medical Centre in Wellington [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/2.%20Lori%20Peters%2C%20NP%20and%20advanced%20HIP%20at%20Mahitahi%20Hauora%2C%20and%20Jasper%20Nacilla%2C%20NP%20at%20The%20Terrace%20Medical%20Centre%20in%20Wellington%20CR%20Simon%20Maude.jpg?itok=sUfbsSF1)
![Ministry of Social Development health and disability coordinator Liz Williams, regional health advisors Mary Mojel and Larah Takarangi, and health and disability coordinators Rebecca Staunton and Myint Than Htut [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/3.%20Ministry%20of%20Social%20Development%27s%20Liz%20Williams%2C%20Mary%20Mojel%2C%20Larah%20Takarangi%2C%20Rebecca%20Staunton%20and%20Myint%20Than%20Htut%20CR%20Simon%20Maude.jpg?itok=9ceOujzC)
![Locum GP Helen Fisher, with Te Kuiti Medical Centre NP Bridget Woodney [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/4.%20Locum%20GP%20Helen%20Fisher%2C%20with%20Te%20Kuiti%20Medical%20Centre%20NP%20Bridget%20Woodney%20CR%20Simon%20Maude.jpg?itok=TJeODetm)
![Ruby Faulkner, GPEP2, with David Small, GPEP3 from The Doctors Greenmeadows in Napier [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/5.%20Ruby%20Faulkner%2C%20GPEP2%2C%20with%20David%20Small%2C%20GPEP3%20from%20The%20Doctors%20Greenmeadows%20in%20Napier%20CR%20Simon%20Maude.jpg?itok=B0u4wsIs)
![Rochelle Langton and Libby Thomas, marketing advisors at the Medical Protection Society [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/6.%20Rochelle%20Langton%20and%20Libby%20Thomas%2C%20marketing%20advisors%20at%20the%20Medical%20Protection%20Society%20CR%20Simon%20Maude.jpg?itok=r52_Cf74)
![Specialist GP Lucy Gibberd, medical advisor at MPS, and Zara Bolam, urgent-care specialist at The Nest Health Centre in Inglewood [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/7.%20Specialist%20GP%20Lucy%20Gibberd%2C%20medical%20advisor%20at%20MPS%2C%20and%20Zara%20Bolam%2C%20urgent-care%20specialist%20at%20The%20Nest%20Health%20Centre%20in%20Inglewood%20CR%20Simon%20Maude.jpg?itok=z8eVoBU3)
![Olivia Blackmore and Trudee Sharp, NPs at Gore Health Centre, and Gaylene Hastie, NP at Queenstown Medical Centre [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/8.%20Olivia%20Blackmore%20and%20Trudee%20Sharp%2C%20NPs%20at%20Gore%20Health%20Centre%2C%20and%20Gaylene%20Hastie%2C%20NP%20at%20Queenstown%20Medical%20Centre%20CR%20Simon%20Maude.jpg?itok=Z6u9d0XH)
![Mary Toloa, specialist GP at Porirua and Union Community Health Service in Wellington, Mara Coler, clinical pharmacist at Tū Ora Compass Health, and Bhavna Mistry, specialist GP at Porirua and Union Community Health Service [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/9.%20Mary%20Toloa%2C%20Porirua%20and%20Union%20Community%20Health%20Service%20in%20Wellington%2C%20Mara%20Coler%2C%20T%C5%AB%20Ora%20Compass%20Health%2C%20and%20Bhavna%20Mistry%2C%20PUCHS%20CR%20Simon%20Maude.jpg?itok=kpChr0cc)