Respiratory physician Lutz Beckert considers chronic obstructive pulmonary disease management, including the prevention of COPD, the importance of smoking cessation and pulmonary rehabilitation, and the lifesaving potential of addressing treatable traits. He also discusses the logic of inhaler therapy, moving from single therapy to dual and triple therapy when indicated, as well as other aspects of management
What does quality care for people with melanoma look like in New Zealand?
What does quality care for people with melanoma look like in New Zealand?
Here at New Zealand Doctor Rata Aotearoa we are on our summer break! While we're gone, check out Summer Hiatus: Stories we think deserve to be read again! This article was first published on 16 March 2022.
In this column, dermatologist Amanda Oakley summarises the Quality Statements to Guide Melanoma Diagnosis and Treatment in New Zealand, focusing on the statements relevant to those working in primary care
- Dermatoscopy is an essential skill for primary care practitioners to help in early detection of melanoma when undertaking full-body skin checks.
- Identify patients at high risk of melanoma due to older age, fair skin, sun damage, previous melanoma or other skin cancer, many naevi or immunosuppression.
- Lesions suspicious of melanoma are excised with a 2mm clinical margin.
This article has been endorsed by the RNZCGP and has been approved for up to 0.25 CME credits for continuing professional development purposes (1 credit per learning hour). To claim your credits, log in to your RNZCGP dashboard to record this activity in the CME component of your CPD programme.
Nurses may also find that reading this article and reflecting on their learning can count as a professional development activity with the Nursing Council of New Zealand (up to 0.25 PD hours).
The Quality Statements to Guide Melanoma Diagnosis and Treatment in New Zealand were launched by MelNet at the online 2022 New Zealand Melanoma Summit on 12–13 February (https://melanomasummit.com).
All health professionals in New Zealand should be familiar with its contents and aim to follow current best practice and reduce inequities. The statements are based on evidence or, when evidence is lacking, on expert consensus. Each of the 23 statements is backed up by the rationale and includes good practice points supported by references.
If you are in primary care, please download the statements document from the MelNet website (tinyurl.com/GuideMelanoma) and keep a copy readily available for reference, although note that it will be updated twice yearly to reflect the latest evidence.
1.1: Prevention and early detection of melanoma
As melanoma in New Zealand is predominantly due to ultraviolet radiation, we need to raise awareness of the damage done by solar exposure and tanning devices in all skin types and ethnicities. Exposure to UV radiation should be limited and sunburn avoided.
The danger of UV radiation is reported as the UV Index. If it is over 3 (September to April), people should be advised to limit time outdoors, choose shade, protect their eyes with wrap-around sunglasses, and protect their skin with long sleeves, a collar and a wide-brimmed hat. Broad-spectrum and water-resistant sunscreen with a sun protection factor of at least 50 should be reapplied every two hours while outdoors during the day.
Although dark skin is less prone to melanoma, Māori and other ethnic minorities are likely to be diagnosed with thicker melanoma with poorer survival than non-Māori. Early detection reduces the chance of a poor outcome; long-term survival depends on the thickness of the melanoma at the time of excision. Many forms of melanoma can be identified when in situ (non-invasive).
Encourage your adult patients – especially those over age 50 – to examine their own skin (with the help of a partner) and to seek advice from a health professional about any suspicious lesion. Explain they should expect a full-body skin check using dermatoscopy.
1.2: Training of primary healthcare professionals
Most melanomas are spotted or confirmed in primary care; thus, it is essential that primary care professionals have the competence to diagnose them and know what to do. In 2022, patients with melanoma can expect their examination to include dermatoscopy. The fundamental skills should be included as part of the General Practice Education Programme.
If you care for patients with melanoma or you undertake skin checks, the good practice points for quality statement 1.2 expect you to:
- know how to assess the patient’s risk of melanoma
- be alert for lesions with malignant features (and become familiar with the appearance of benign keratoses and melanocytic naevi – refer back to “Dermatology”, New Zealand Doctor, 12 May and 1 September 2021)
- be trained in the basic use of a dermatoscope and to refresh your knowledge
- arrange a full-body skin check for a patient at risk or presenting with a lesion of concern.
1.3: People at increased risk of melanoma
Anyone can get melanoma – most adults are at average risk and children and very dark-skinned individuals are at lower risk. It’s useful to identify people at higher risk to encourage them to present early with concerns about a skin lesion and schedule skin checks at appropriate intervals.
The usual reasons for high risk are increased age, fair skin and sun damage. Individuals may also have had a previous melanoma, familial melanoma (rare), many melanocytic naevi, giant congenital naevus, previous keratinocyte cancer or immunosuppression (especially organ transplant recipients).
A validated model for individuals to assess their risk of melanoma is provided by the Melanoma Institute Australia (melanomarisk.org.au). New Zealanders should enter Tasmania as the “Region of Australia most lived in”
People who have had melanoma, two or more first-degree relatives who had melanoma before they were 40, or many moles (especially if these are atypical) should be under the long-term care of a healthcare professional who is competent in skin surveillance using dermatoscopy and digital dermatoscopy. Consider baseline total-body photography and high-quality sequential digital dermatoscopy imaging annually for these patients.
2.1: Timely access to services
Skin lesions that are highly suspicious of melanoma are irregular in structure and colour and are not seborrhoeic keratoses; change may have been observed. Advocate for your patient when referring to secondary care with confirmed invasive melanoma or a lesion suspicious of invasive melanoma. They will likely be anxious.
Wherever the patient resides, whatever their ethnicity, and whether they are receiving publicly funded or private healthcare, the quality statements expect a referral to be followed by:
- completion of wide local excision for confirmed melanoma within 62 days, and within 31 days of the decision to treat (eg, receipt of biopsy report of melanoma)
- first specialist assessment of a high-suspicion invasive or metastatic melanoma within 14 days
- diagnostic excision for a lesion suspicious of melanoma within 14 days of specialist assessment or image-based triage.
In many parts of New Zealand, referrals to the local DHB and responses are electronic, sometimes in the form of teledermatology. High-quality macroscopic and dermatoscopic images of the lesion of concern are encouraged or required.
3.1: Patient access to trained healthcare professionals
All patients should have access to a melanoma nurse coordinator and a multidisciplinary team, including a healthcare professional trained in:
- early detection and diagnosis of melanoma, including the use of dermatoscopy
- triage and referral of suspicious or tricky lesions
- surgical management.
In primary care, patients should have access to a designated, trained GP who can assess the patient history, examine the whole skin surface, recognise benign and suspicious lesions, and who uses dermatoscopy.
Short-term monitoring of low-suspicion flat lesions is over three months and with the aid of dermatoscopic images. Suspicious thickened lesions should be referred or excised.
3.2: Excision of melanocytic lesions
The preferred biopsy technique for excision of melanocytic lesions suspected of being melanoma is a narrow complete excision biopsy, with 2mm margins, that encompasses the entire lesion and is of sufficient depth to avoid transection at the base. All tissue specimens are sent for formalin-fixed paraffin-embedded histopathology.
Diagnostic excision can be undertaken in primary care providing the health professional has the training and skills to do so.
5.1: Re-excision of histologically confirmed melanomas
Histologically confirmed melanomas are re-excised, with additional clinical margins determined by Breslow thickness (see table). Lesions with American Joint Committee on Cancer (AJCC) histological staging of T1b (Breslow thickness 0.8mm with ulceration) or higher are referred to an appropriately trained and experienced surgical specialist. The designation of such a specialist varies by region.
Re-excision of melanoma in situ to 5–10mm clinical margins, and re-excision of AJCC T1a (Breslow thickness 0.8mm without ulceration) cases of melanoma to 10mm clinical margins, can be performed as a local-anaesthetic procedure by either an appropriately trained and experienced primary healthcare doctor or a melanoma specialist.
5.2: Desmoplastic/neurotropic melanoma
5.6: Patients with loco-regionally recurrent, locally advanced and stage IV melanoma
These forms of melanoma should be discussed at a multidisciplinary meeting, whatever tumour stage is reported, on referral to secondary care.
6.1: Clinical follow-up and surveillance
6.2: Patient self-examination
7.1: Supportive care
GPs may be asked, or expected, to follow up patients with melanoma to detect recurrence early (ask about symptoms and examine the excision scar site, surrounding skin and local lymph nodes), to detect new primary melanoma (perform a full-body skin check with dermatoscopy), to teach them how to self-examine their skin, and to provide psychosocial support and information about their disease and its treatment (refer them on if needed).
Patients with additional risks, such as multiple melanomas, familial melanoma, numerous naevi, older age, very fair skin or history of keratinocyte cancers, should be offered lifelong annual or biennial skin checks.
Follow-up protocols for assessing disease recurrence or metastatic spread are as follows:
- stage 0 melanoma in situ – biennial dermatoscopic skin check for at least 10 years
- stage IA melanoma – assessed annually for 10 years
- stage IB and IIA melanoma – assessed six-monthly for two years, then annually until the 10th anniversary
- stage IB and above melanoma with no sentinel node biopsy – six-monthly ultrasound of draining node fields for two years
- stage IIB–C and IIIA–D melanoma – assessed four-monthly for two years, six-monthly in the third year and annually thereafter until the 10th anniversary
- stage IV melanoma – as for stage III, with additional visits as per clinical requirements.
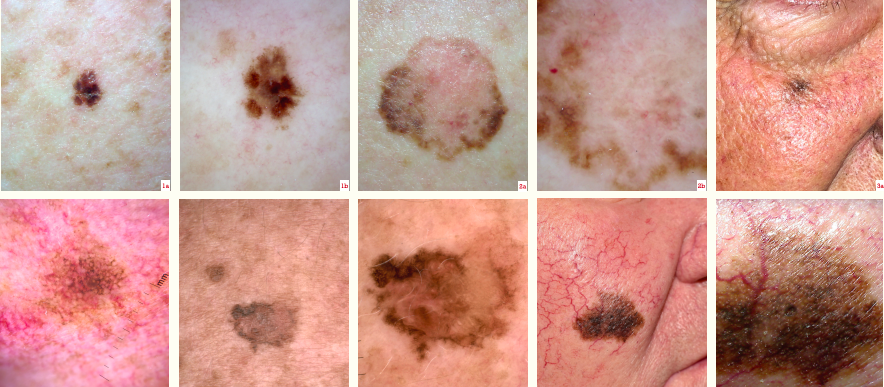
Each “a” image is the clinical view, and each “b” image is dermatoscopy
Figure 1. Severely atypical naevus
Figure 2. Superficial spreading melanoma in situ
Figure 3. Melanoma in situ (lentigo maligna)
Figure 4. Lentiginous melanoma in situ
Figure 5. Lentigo maligna melanoma 0.2mm
Amanda Oakley, CNZM, is a specialist dermatologist at Waikato Hospital, an adjunct associate professor at Waikato Clinical Campus, and founder of DermNetNZ.org
You can use the Capture button below to record your time spent reading and your answers to the following learning reflection questions:
- Why did you choose this activity (how does it relate to your professional development plan learning goals)?
- What did you learn?
- How will you implement the new learning into your daily practice?
- Does this learning lead to any further activities that you could undertake (audit activities, peer discussions, etc)?
MelNet. Quality Statements to Guide Melanoma Diagnosis and Treatment in New Zealand. Christchurch, NZ: Melanoma Network of New Zealand; 2021. https://www.melnet.org.nz/resources/quality-statements-to-guide-melanoma-diagnosis-and-treatment-in-new-zealand








![Barbara Fountain, editor of New Zealand Doctor Rata Aotearoa, and Paul Hutchison, GP and senior medical clinician at Tāmaki Health [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/Barbara%20Fountain%2C%20editor%20of%20New%20Zealand%20Doctor%20Rata%20Aotearoa%2C%20and%20Paul%20Hutchison%2C%20GP%20and%20senior%20medical%20clinician%20at%20T%C4%81maki%20Health%20CR%20Simon%20Maude.jpg?itok=-HbQ1EYA)
![Lori Peters, NP and advanced health improvement practitioner at Mahitahi Hauora, and Jasper Nacilla, NP at The Terrace Medical Centre in Wellington [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/2.%20Lori%20Peters%2C%20NP%20and%20advanced%20HIP%20at%20Mahitahi%20Hauora%2C%20and%20Jasper%20Nacilla%2C%20NP%20at%20The%20Terrace%20Medical%20Centre%20in%20Wellington%20CR%20Simon%20Maude.jpg?itok=sUfbsSF1)
![Ministry of Social Development health and disability coordinator Liz Williams, regional health advisors Mary Mojel and Larah Takarangi, and health and disability coordinators Rebecca Staunton and Myint Than Htut [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/3.%20Ministry%20of%20Social%20Development%27s%20Liz%20Williams%2C%20Mary%20Mojel%2C%20Larah%20Takarangi%2C%20Rebecca%20Staunton%20and%20Myint%20Than%20Htut%20CR%20Simon%20Maude.jpg?itok=9ceOujzC)
![Locum GP Helen Fisher, with Te Kuiti Medical Centre NP Bridget Woodney [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/4.%20Locum%20GP%20Helen%20Fisher%2C%20with%20Te%20Kuiti%20Medical%20Centre%20NP%20Bridget%20Woodney%20CR%20Simon%20Maude.jpg?itok=TJeODetm)
![Ruby Faulkner, GPEP2, with David Small, GPEP3 from The Doctors Greenmeadows in Napier [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/5.%20Ruby%20Faulkner%2C%20GPEP2%2C%20with%20David%20Small%2C%20GPEP3%20from%20The%20Doctors%20Greenmeadows%20in%20Napier%20CR%20Simon%20Maude.jpg?itok=B0u4wsIs)
![Rochelle Langton and Libby Thomas, marketing advisors at the Medical Protection Society [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/6.%20Rochelle%20Langton%20and%20Libby%20Thomas%2C%20marketing%20advisors%20at%20the%20Medical%20Protection%20Society%20CR%20Simon%20Maude.jpg?itok=r52_Cf74)
![Specialist GP Lucy Gibberd, medical advisor at MPS, and Zara Bolam, urgent-care specialist at The Nest Health Centre in Inglewood [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/7.%20Specialist%20GP%20Lucy%20Gibberd%2C%20medical%20advisor%20at%20MPS%2C%20and%20Zara%20Bolam%2C%20urgent-care%20specialist%20at%20The%20Nest%20Health%20Centre%20in%20Inglewood%20CR%20Simon%20Maude.jpg?itok=z8eVoBU3)
![Olivia Blackmore and Trudee Sharp, NPs at Gore Health Centre, and Gaylene Hastie, NP at Queenstown Medical Centre [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/8.%20Olivia%20Blackmore%20and%20Trudee%20Sharp%2C%20NPs%20at%20Gore%20Health%20Centre%2C%20and%20Gaylene%20Hastie%2C%20NP%20at%20Queenstown%20Medical%20Centre%20CR%20Simon%20Maude.jpg?itok=Z6u9d0XH)
![Mary Toloa, specialist GP at Porirua and Union Community Health Service in Wellington, Mara Coler, clinical pharmacist at Tū Ora Compass Health, and Bhavna Mistry, specialist GP at Porirua and Union Community Health Service [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/9.%20Mary%20Toloa%2C%20Porirua%20and%20Union%20Community%20Health%20Service%20in%20Wellington%2C%20Mara%20Coler%2C%20T%C5%AB%20Ora%20Compass%20Health%2C%20and%20Bhavna%20Mistry%2C%20PUCHS%20CR%20Simon%20Maude.jpg?itok=kpChr0cc)