Respiratory physician Lutz Beckert considers chronic obstructive pulmonary disease management, including the prevention of COPD, the importance of smoking cessation and pulmonary rehabilitation, and the lifesaving potential of addressing treatable traits. He also discusses the logic of inhaler therapy, moving from single therapy to dual and triple therapy when indicated, as well as other aspects of management
Epilepsy
Epilepsy
Epilepsy is a common neurological condition encountered in general practice. This article, by Suzanne Davis and Elizabeth Walker, discusses recommendations regarding diagnosis and indications for starting anti-seizure medication. It also reviews self-management and lifestyle issues for people with epilepsy
This “How to treat” has been endorsed by the RNZCGP and has been approved for up to 1 credit for continuing professional development purposes (1 credit per learning hour). To claim your CPD credits, complete the assessment at the end of this page, then log in to your Te Whanake dashboard and record this activity under the appropriate learning category.
The College of Nurses Aotearoa (NZ) has endorsed this “How to treat” for 1.5 hours of professional development following completion of the assessment at the end of this page (CNA070).
At the end of the course you should be able to:
- Discuss the diagnosis and classification of epilepsy syndromes
- Identify appropriate anti-seizure medications for different types of epilepsy
- Recognise adverse effects of anti-seizure medications
- Explain the risks related to epilepsy for women of childbearing age
- Discuss the role of primary care in managing patients with epilepsy
This How to Treat may assist with the development of the following domains of competence in the general practice curriculum:
- Domain 1: Communication
- Domain 2: Clinical expertise
- Domain 3: Professionalism
- Domain 4: Scholarship
- Domain 5: Context of general practice
- Domain 6: Management
Epilepsy is a group of disorders defined by the occurrence of epileptic seizures, which are events that arise due to abnormal electrical activity in the brain. Epileptic disorders can present at any age but have peaks of onset in infancy/childhood and in older age.
Epileptic seizures can range from brief behavioural arrests to stiffening and/or jerking of the whole body. The International League Against Epilepsy (ILAE; www.ilae.org) defines epilepsy as:
- at least two unprovoked (or reflex) epileptic seizures occurring more than 24 hours apart
- one unprovoked (or reflex) epileptic seizure and a probability of further epileptic seizures, similar to the general recurrence risk after two unprovoked seizures (at least 60 per cent), occurring over the next 10 years
- diagnosis of an epilepsy syndrome.
For example, a person with tuberous sclerosis who has a single seizure would have a probability of experiencing a second seizure of greater than 60 per cent. A young adult who had a single generalised tonic-clonic seizure, has myoclonic jerks in the mornings, and generalised polyspike discharges with photosensitivity on electroencephalogram (EEG) would have an epilepsy syndrome – juvenile myoclonicepilepsy.
There are multiple causes of epilepsy. In many individuals, it has an underlying genetic cause. This can be due to an abnormality in a single gene or due to the interaction of multiple genes, but it is often not inherited. Epilepsy can also be acquired due to an insult to the brain, such as head injury, hypoxic ischaemic injury (including stroke), infection or immunologically mediated disorders.1,2
A 2017 systematic review and meta-analysis of international studies reporting the prevalence and incidence of epilepsy found the pooled point prevalence of active epilepsy in high-income countries to be 5.49 per 1000 people. The pooled estimate for the incidence of epilepsy in high-income countries was 48.86 per 100,000 people.3
Applying these international estimates to our New Zealand population suggests that approximately 2400 people are diagnosed with epilepsy each year and approximately 27,000 people in New Zealand live with epilepsy. Thus, it is likely that most GPs have patients in their care who have epilepsy.
A recent report of prolonged seizures in patients presenting to Auckland hospitals from 2015 to 2016 found the age-adjusted incidence of patients with seizures lasting 10 minutes or longer to be 22.22 per 100,000 head of population per year. The age-adjusted incidence of longer seizures was higher in Māori (29.31/100,000/year) and Pacific patients (26.55/100,000/year) than in those with European (19.13/100,000/year) or Asian/other descent (17.76/100,000/year).4
The first step in the management of epilepsy is to establish the correct diagnosis. Current guidelines require that the diagnosis of an epileptic seizure be made by a specialist – either a paediatrician or neurologist.
Identify the type of epileptic seizure
A new terminology for describing and classifying epileptic seizures was introduced by the ILAE in 2017.1 It is summarised in Table 1.
An accurate history of events is most important in determining a patient’s seizure type
An accurate history of events is most important in determining a patient’s seizure type. Focal seizures are first defined by the earliest symptom or sign as motor (eg, clonic or atonic) or non-motor (eg, sensory or cognitive). The second step in the definition is determination of altered awareness at any stage in the progression of the seizure event.
For example, in a focal aware motor seizure, the patient is aware and fully oriented to the environment throughout the seizure. In a focal sensory seizure with impaired awareness, the patient experiences a sensory phenomenon, such as an unusual smell, then loses awareness and may have no memory of the event. Note that focal seizures with altered awareness were previously termed “partial complex seizures”.
Another important feature of the new classification is the term “focal to bilateral seizure”. This term replaces the previous “secondarily generalised seizure”.
Often, the onset of an epileptic seizure is not witnessed. In this case, a seizure with bilateral motor signs, such as tonic or tonic-clonic movements, is classified as an “unknown” seizure type as the description of the onset of the event is not available.
Identify the type of epilepsy
The next step, after diagnosis of the type of seizure, is diagnosis of the type of epilepsy. Epilepsy syndromes were also reclassified by the ILAE in 2017, into four types: focal, generalised, combined generalised and focal, and unknown.2 These epilepsy syndromes are defined according to seizure type, age of onset and comorbidities, such as cognitive and behavioural disorders. The EEG and brain imaging findings (discussed later) may also play a role in identification of an epilepsy syndrome.
Confirm the diagnosis
The diagnosis of epilepsy carries significant implications for the patient, particularly with respect to driving, education and employment. It is imperative to be confident in the diagnosis of an epileptic disorder before recommending and commencing treatment with an anti-seizure medication (ASM). The features of some epileptic and non-epileptic events are summarised in Table 2.
People who witness recurrent seizures should be encouraged to record the events on their phones
Acute symptomatic seizures
Acute symptomatic seizures have a direct reversible cause and do not indicate that seizures will recur when the immediate cause is removed. Examples include drug exposure (eg, tramadol or alcohol), hypoglycaemia, electrolyte disorders, acute head injury, stroke, cerebral hypoxia, central nervous system infections and autoimmune encephalitis. The seizures may be managed acutely with an ASM, but medication is not necessarily continued after the patient has recovered from the underlying condition.
Febrile seizures
The ILAE defines a febrile seizure as a seizure occurring in childhood after one month of age and associated with a febrile illness not caused by any infection of the central nervous system. It occurs without previous neonatal seizures or previous unprovoked seizures and does not meet the criteria for other symptomatic seizures.
A simple febrile seizure is a generalised tonic-clonic seizure under 10 minutes in duration with no recurrence within 24 hours or within the same febrile illness. A complex febrile seizure may have some focal features, be longer than 10 minutes in duration, and two or more may occur within 24 hours or within the same febrile illness.
Hospital admission should be considered after the first febrile seizure if the child is under 18 months of age, has a complex febrile seizure, has no identified focus of infection, or where there is high parental or carer anxiety.
The risk of recurrence after a febrile seizure is 30–40 per cent and is higher in infants under 12 months (50 per cent) than in children over three years (20 per cent). There is a low but increased risk of epilepsy after a febrile seizure (3 per cent overall). The risk is higher (up to 10 per cent) if there is abnormal neurological examination, a family history of epilepsy in a first-degree relative, and after a complex febrile seizure.
Regular or intermittent ASM is not recommended for febrile seizures. Infants and children should be referred to a paediatrician if they have more than three discrete febrile seizure events, if they are younger than six months or older than six years, if the seizures last longer than 30 minutes or they have focal features.
Investigate the cause
The first step in the identification of the cause of an epileptic disorder is the accurate definition of the type of seizure(s) based on a detailed history. This includes review of video recordings of typical events if these are available.
As so many people carry smart phones, video recording of seizure events is now commonplace. People who witness recurrent seizures should be encouraged to record the events on their phones. It is important to remember that in most videos, only the second half or end of an event is recorded.
Family history
Genetic causes of epilepsy may or may not be associated with inheritability, and the family history may be non-contributary. On the other hand, many genetic epilepsies (eg, childhood absence epilepsy and juvenile myoclonic epilepsy) are associated with an increased incidence of epileptic seizures in other family members.
Electroencephalogram
The EEG is often helpful in determining whether an epileptic disorder is focal or generalised; some EEG findings will point to a specific epilepsy syndrome. In New Zealand, an EEG is recommended after the first epileptic seizure and is ordered by the specialist who carries out the initial diagnostic evaluation.
The EEG cannot be used to identify a seizure event as epileptic because abnormalities defined as epileptiform can be present in people who do not have epilepsy, especially in children. On the other hand, many people with epilepsy will have a normal EEG.
In New Zealand, a routine EEG is often performed after sleep deprivation to increase the likelihood of finding diagnostic abnormalities. The inclusion of a period of natural sleep in the EEG recording also increases the diagnostic yield.
Brain imaging
MRI is the technique of choice in investigation of an epileptic disorder. It is recommended for any patient under the age of two presenting with an epileptic seizure, following a focal epileptic seizure, in the presence of focal neurological signs, and in patients with specific comorbidities, such as cognitive and behavioural disorders.
CT imaging is not sufficient to investigate the cause of an epileptic disorder. A CT scan is indicated when acute focal pathology (eg, trauma, haemorrhage or stroke) is suspected in the setting of an acute presentation of an epileptic seizure and an MRI is not immediately available.
Brain imaging is not necessary when a definite diagnosis of a generalised genetic epilepsy, such as childhood absence epilepsy or juvenile myoclonic epilepsy, is made.
In general, treatment is considered when there is evidence of recurrent seizures and is usually initiated after a second epileptic seizure. In some epileptic disorders, depending on the identification of the cause of the epilepsy, treatment is indicated after the first seizure when the probability of subsequent recurrent seizures is greater than 60 per cent.
Recurrence risk after the first epileptic seizure varies, with the highest risk (up to 90 per cent) in people with epileptic discharges in the EEG and focal neurological deficits. In people with a normal EEG and no identifiable cause for the epilepsy, the recurrence risk is lower (13–40 per cent). Overall, the risk of a second seizure is 30–40 per cent and is greatest in the first 12 months, falling to less than 10 percent after two years.
In New Zealand, it is recommended that an evaluation be made by a specialist after the first suspected epileptic seizure. Current recommendations state that this should occur within three weeks of the initial presentation. Many DHBs have established first-seizure clinics or have made other arrangements for patients to be seen in a timely fashion after the first seizure.
It is expected that the specialist completes a diagnostic evaluation and orders an EEG if a probable epileptic seizure is identified. A decision regarding brain imaging and a choice of first-line ASM is then made. In many circumstances, the patient will present to their GP with a subsequent seizure, and the ASM can be commenced as recommended by the specialist.
Patients are encouraged to practice self-management, including good compliance with the medication regimen, if education regarding the justification for treatment and expectations about possible adverse effects is available from the onset of treatment. There is excellent information regarding epilepsy and its treatment available online that should be provided to the patient and family as appropriate (see the patient information resources listed at the end of this article).
In most circumstances, this protocol of delaying treatment until a diagnostic assessment has been completed is safe and effective. There is evidence that the timing of onset of treatment does not alter the long-term prognosis for seizure control. Factors that predict outcome include the response to the appropriately selected first-line medication and the number of seizures occurring in the first six months from presentation.
Which medication to choose?
Treatment should include the most effective medication for achieving complete seizure control with the least adverse effects. An inappropriately chosen medication may be ineffective and produce adverse effects that are more disabling than the seizures themselves. The choice of treatment should be guided by seizure and epilepsy type (Table 3).
A second-line medication is indicated when first-line medication has clearly failed
Focal epilepsies
Carbamazepine, lamotrigine and levetiracetam have been shown to be equally effective as first-line therapy for focal seizures, with lamotrigine having a better adverse effects profile. Levetiracetam has the advantage of a more rapid titration than carbamazepine or lamotrigine, but it has the disadvantage of causing unacceptable psychiatric side effects of behavioural agitation, depression and anxiety in approximately 10 per cent of patients.
Generalised epilepsies
Sodium valproate has been shown to be the most effective medication for first-line therapy in genetic generalised epilepsies, such as juvenile myoclonic epilepsy. However, as sodium valproate is associated with the highest risk of foetal malformations and neurodevelopmental disorders in children exposed in utero, it is not indicated as first-line therapy for generalised epilepsies in women of childbearing age. Levetiracetam or lamotrigine are the most appropriate first-line therapies for these patients.
Rescue medications
Buccal midazolam
Patients who have experienced prolonged seizures of greater than five minutes should be prescribed midazolam, taken by the buccal or nasal route. Midazolam is available in New Zealand in plastic ampoules (15mg/5ml). Training is necessary for caregivers and family who will administer the midazolam.
Rectal diazepam
Diazepam administered rectally has been used in the past as a rescue medication. It has been shown to be less effective than buccal midazolam in stopping prolonged seizures and has a higher incidence of respiratory depression.
Oral clobazam
Clobazam can be administered orally after a seizure when the person habitually experiences seizures in clusters over several hours, especially if there has been a provocation, such as sleep deprivation. Clobazam can also be taken as a single daily dose on several consecutive days during a seizure cluster (eg, perimenstrually in women who experience catamenial seizures).
Medication-resistant epilepsy
Approximately 60 per cent of people with newly diagnosed epilepsy become seizure free on first-line medication. If seizures recur, it may be because the diagnosis of epilepsy was incorrect, an inappropriate medication was chosen for the epilepsy syndrome or the person is not compliant with the medication regimen. In some cases, other medications, drugs or alcohol may cause further seizures or there may be an undetected epileptogenic cerebral lesion, such as a tumour.
Failure of a first-line medication to control seizures may be an indication to repeat the EEG to confirm the epilepsy syndrome, and to review or repeat brain imaging with MRI. A second-line medication is indicated when first-line medication has clearly failed. However, up to 30 per cent of patients will have medication-resistant epilepsy, which is defined as a failure of two tolerated and appropriately chosen and used ASM schedules (whether as monotherapies or in combination) to achieve sustained seizure freedom.
Some people with medication-resistant epilepsy have a developmental and epileptic encephalopathy, with cognitive and behavioural disorders in addition to epilepsy. Any person who has failed two appropriately chosen and tolerated ASMs should be referred to a specialist – paediatrician or neurologist – for diagnostic re-evaluation and consideration of non-medical treatment, such as diet or epilepsy surgery.
It is important to advise all girls and women of the issues related to epilepsy and pregnancy when ASMs are first prescribed
It should be assumed that every patient taking ASMs may experience some side effects, mostly by causing sedation or mood changes. This should be taken into consideration when a decision is made to treat the disorder, and good patient self-management requires an understanding of how side effects can be managed.
Many side effects are dose related, predictable and can be minimised by a gradual escalation in the dose. Carbamazepine is a typical example of a medication that should be commenced at a low dose (100–200mg/day in an adult) and increased in increments of 100–200mg over the course of two weeks as it increases its own metabolism over this time period. Older people are more susceptible to medication side effects due to altered pharmacokinetics.
Adverse effects and monitoring
Rare idiosyncratic medication reactions mostly occur in the first few weeks of treatment, and they can be severe. Rash is the most common and occurs most often with carbamazepine and lamotrigine. The incidence of rash is reduced by slow introduction of the medication. A rash occurring between two weeks and two months of medication introduction is an indication to discontinue the medication immediately. Most rashes will resolve over days when the medication is discontinued. Life-threatening ASM hypersensitivity with multi-organ failure occurs rarely – in up to 4.5 per 10,000 people exposed.
Mild blood dyscrasias (eg, leucopenia with carbamazepine and thrombocytopenia with sodium valproate) are common and no intervention is needed. Severe blood dyscrasias are rare, occurring in up to six per 10,000 people exposed. Routine monitoring of blood count is not recommended as there is no evidence that this reduces the risk.
Hyponatraemia is common in people taking carbamazepine, especially in children, older people and those with restricted dietary salt intake. Monitoring of electrolytes and liver function should depend on clinical symptoms and is not recommended as routine in asymptomatic people taking ASMs. Enzyme induction is common with carbamazepine and phenytoin, resulting in elevation of enzymes, such as gamma-glutamyl transferase. This is not an indication to change or cease therapy.
Long-term treatment with ASMs may reduce bone density, especially in people with limited mobility. There are no current guidelines regarding routine monitoring of bone density, but prophylactic vitamin D should be considered for people at highest risk.
Psychiatric comorbidity
Depression is the most common psychiatric comorbidity in people with epilepsy – it occurs in up to 45 per cent of patients at some stage. All ASMs are associated with behavioural side effects, and some (particularly levetiracetam and topiramate) have a higher incidence of significant psychiatric adverse effects, including depression.
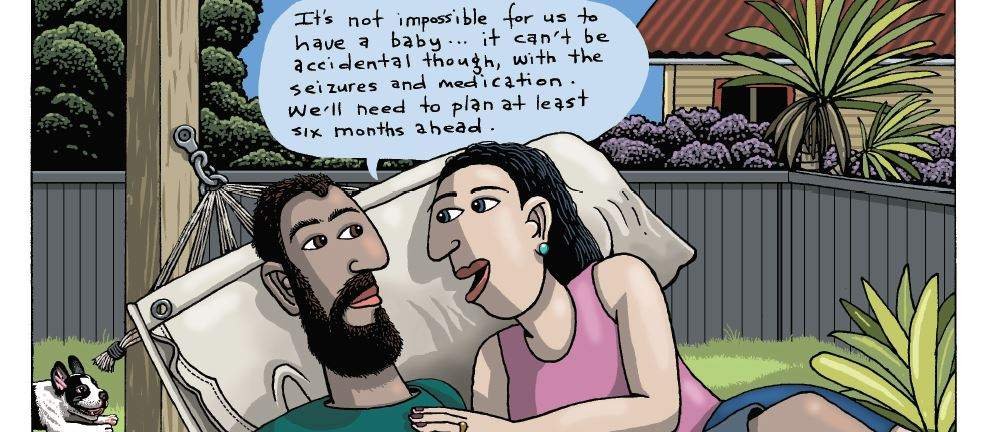
Women of childbearing age
Women of childbearing age should be fully informed of the risks to the foetus with any of the medications prescribed, as well as the risks to both herself and her foetus from uncontrolled seizures during pregnancy. As about half of pregnancies are unplanned, it is important to advise all girls and women of the issues related to epilepsy and pregnancy when ASMs are first prescribed.
Women are advised to use two forms of contraception when taking ASMs and should be assessed and managed by a neurologist before planning a pregnancy. Daily folic acid at a dose of 5mg per day is recommended in all women of childbearing age with epilepsy.
Educational resources about the use of ASMs in pregnancy are available for both prescribers and patients (see the lists at the end of this article), including two booklets prepared by ACC (go to: acc.co.nz/treatmentsafety).
Hormonal contraception
Enzyme-inducing ASMs (eg, carbamazepine and topiramate) reduce the contraceptive effect of oral contraceptives. There is evidence that lamotrigine induces the metabolism of the progestin levonorgestrel. If an oral contraceptive is used with an enzyme-inducing ASM, a higher oestrogen formulation is recommended (eg, 50μg). Even at the higher dose, contraception cannot be guaranteed, and additional protection is needed.
Progesterone-only oral contraceptives are likely to be ineffective when enzyme-inducing ASMs are taken. On the other hand, depot medroxyprogesterone acetate injections appear to be effective but need to be given more frequently. Use of additional forms of contraception, such as intrauterine devices, is recommended.
It is also important to be aware that lamotrigine levels are reduced by oral contraceptives. Women taking lamotrigine for epilepsy need to have levels monitored when oral contraceptives are commenced, and signs of toxicity should be monitored when oral contraceptives are discontinued.
Anti-seizure medication during pregnancy
Uncontrolled generalised tonic-clonic seizures expose both the pregnant mother and foetus to significant risk for morbidity and mortality. For some women, pregnancy exposes them to a higher risk for seizures. Lamotrigine levels are significantly reduced during the second trimester of pregnancy, requiring close monitoring of the dose and blood levels. Another frequent cause of breakthrough seizures during pregnancy is self-manipulation of the medication dose.
ASM exposure to the foetus is known to increase the risk of major foetal malformations and, in some cases, also increase the risk of later developing neurodevelopmental disorders, including autistic spectrum disorder. For some ASMs, such as sodium valproate, the risk to the foetus is dose related:
- Sodium valproate at doses greater than 1500mg/day exposes the foetus to the highest risk for foetal malformations, such as spina bifida, cleft palate and heart defects – 24 per cent risk of babies are affected, compared with 2–3 per cent of babies unexposed to ASMs and 4–7 per cent of babies exposed to any ASM.
- Sodium valproate at doses greater than 800mg/day are associated with an increased risk for childhood developmental delays, and autistic spectrum disorder occurs in 4–15 per cent of children exposed in utero compared with 2–7 per cent of children unexposed to ASMs. Children exposed to sodium valproate in utero are eight times more likely to need extra help in school than other children.
Carbamazepine, lamotrigine and levetiracetam are associated with a significantly lower risk to the foetus. Monotherapy is recommended during pregnancy, and there is substantial evidence that polytherapy with sodium valproate is associated with higher risks.
It is recommended that women with epilepsy who plan a pregnancy are referred for specialist evaluation one year, but no less than six months, before discontinuing contraception so gradual transition to a more appropriate medication regimen can occur.
Stopping anti-seizure medication
The timing of a decision to discontinue ASMs will depend on the specific epilepsy syndrome as this will determine the prognosis for seizure freedom when off medication. Some epilepsies may require long-term ASM therapy. When a person with epilepsy has been seizure free on medication for two or more years, it is customary to begin a discussion regarding discontinuation of medication.
The balance between adverse effects of continued medication and the risk of further seizures should be discussed. It is reasonable to refer the patient to a specialist for this discussion.
Most ASMs can be tapered over two months. However, several ASMs, such as phenobarbital and clonazepam, will require a longer period of dose reduction (up to six months). The patient must cease driving during the taper and for three months afterwards.
A person taking medication for epilepsy should have a review of their management at least annually
The GP and practice nurses play an important role in supporting self-management in people with epilepsy. This includes actions that enhance adherence to a medication regimen and liaising between patients and community, educational or other health services, particularly for patients with cognitive, psychiatric and multiple comorbidities.
A person taking medication for epilepsy should have a review of their management at least annually, even if seizure free, but especially if seizures are recurring. Even as few as one seizure per year can cause major disruption to social, educational and employment opportunities, and will prevent the person from legally driving a vehicle.
The annual review will determine medication compliance and assess any barriers to full compliance, confirm appropriate contraception by two methods and discuss any plans for pregnancy in women of childbearing age, assess any adverse effects of medications and determine if there are any important medication interactions.
At the review, the patient’s management of risks in their everyday life should be discussed. In addition, the review should note any barriers to participation in education or employment and reinforce knowledge of the regulations regarding driving. The patient should be given information about the services of Epilepsy New Zealand if they are not already participating.
A person with epilepsy who continues to have seizures, even as infrequently as once per year, and is compliant with the recommended medication regimen should be referred to a paediatrician or neurologist.
Minimising risk of injury
People with epilepsy should be aware of the risks they might be exposed to during a seizure. Preventable injuries and deaths during seizures are not uncommon. Drowning is the most common cause of death caused by a seizure. Risk of drowning can be minimised by advising the patient to shower rather than take a bath, and to swim with one-on-one supervision from a responsible adult who is aware of their epilepsy. Bicycle riding, especially around traffic, and climbing to places about one metre or more off the ground should be avoided.
Driving after a seizure
Seizures are a rare cause of traffic accidents, but the regulations regarding driving are clearly laid out by the Waka Kotahi NZ Transport Agency. The regulations should be brought to the attention of any patient who is driving, or intends to drive, after the first seizure.
For Class 1 licences, a single seizure means a person will need to stop driving for 12 months. In exceptional circumstances, the 12-month stand-down period may be reduced if there is a clearly identified, non-recurring cause. This can be reviewed in consultation with a neurologist.
When a person with epilepsy is treated with an ASM, they are required to be free of a seizure for 12 months before they are permitted to drive. There is also a stand-down period from driving if the medication is changed or discontinued.
There is an exception for people who have only nocturnal seizures – they may drive if they have a stable pattern of seizures at night and are free of awake seizures for 12 months.
For other classes of licence and endorsements, a person with a seizure or seizure disorder is considered permanently unfit to drive.
Sudden unexpected death in epilepsy
People with epilepsy have a small but real risk of death. It is important that patients and their caregivers are educated regarding this risk at the time of diagnosis.
Sudden unexpected death in epilepsy is defined as sudden, unexpected, witnessed or unwitnessed, non-traumatic and non-drowning death in patients with epilepsy, with or without evidence for a seizure and excluding documented status epilepticus, in which post-mortem examination does not reveal a structural or toxicological cause of death.
SUDEP is reported to be the cause of 2–18 per cent of all deaths in people with epilepsy. The overall incidence is one in 4500 patient-years in children and one in 1000 patient-years in adults. The cause of SUDEP is unknown but is theorised to be due to respiratory suppression followed by cardiac arrest in the postictal period of a tonic-clonic seizure.
The main risk factor for SUDEP is the presence of tonic-clonic seizures – one or two tonic-clonic seizures per year increases the risk five fold, while more than three per year results in a 15-fold increased risk compared with those who are seizure free. Other risk factors include age (highest risk in the 18–25 age group), uncontrolled epilepsy, nocturnal seizures and intellectual disability.
Community services for people with epilepsy
Epilepsy New Zealand is an organisation that has a nationwide focus and employs support workers (also knows as field staff and educators) across 12 field offices. These field offices deliver services through paid staff and volunteers. Programmes provided by epilepsy New Zealand include advocacy, awareness, research, information and education, and support services.
People with epilepsy can engage with Epilepsy New Zealand casually by attending a seminar or contacting an epilepsy educator. People may also be more actively involved by joining as a member. It is recommended that all patients are provided with information regarding community support services at the time of diagnosis of their epilepsy.
A timely second opinion
Presentation and history
Susan is a 52-year-old woman who consults her GP about a recent probable seizure and her disallowed driving. She has no past history of seizures. Susan recently had herpes ophthalmicus complicated by acute glaucoma, for which she received aggressive therapy, including timolol maleate ophthalmic solution. She has hypertension treated with a diuretic.
Recent seizure event
On the day of the event, Susan went with her husband to a movie. She had been feeling a little unwell before leaving home. When she was watching the movie, she began to feel nauseated and sweaty. Her husband describes her as moaning, then becoming rigid with her right arm elevated for about one minute. She then slumped and her head dropped onto his shoulder. She was incontinent of urine.
The ambulance was called. Susan recalls walking in the aisle to the ambulance, and her husband says she did not appear confused. Her blood pressure, recorded at the scene, was 60/80mmHg.
In the emergency department, Susan’s head CT scan was normal. Routine blood tests, including electrolytes, were also normal. A diagnosis of seizure was made, and she was instructed not to drive for 12 months.
Referral
The driving restriction is significant as Susan is a sales representative. Her GP decides to refer her to a neurologist for an opinion.
Diagnosis
The neurologist makes a confident diagnosis of a convulsive syncope based on the preceding symptoms of nausea and sweating, the low blood pressure on initial assessment and relatively rapid recovery without confusion. The event was more severe than a typical syncope as Susan was wedged upright in her seat. Urine incontinence can occur in the context of prolonged cerebral hypoxia.
Predisposing factors were the beta-blocker used for glaucoma and the diuretic for hypertension. Syncope is confirmed by a cardiologist and the diuretic is stopped. Susan is able to return to driving after two months.
Day and night seizures
Presentation and assessment
Jen is a 20-year-old woman who visits her GP for advice. For the last two to three years, she has had spells when she blanks out and loses track of conversations. She also has muscle twitches in her hands in the mornings. She awoke on the morning before this visit with a sore mouth and found she had bitten her tongue during her sleep. Her muscles also felt sore.
Jen appears normal except for bruising on one side of her tongue. Her bitten tongue and sore muscles suggest she had a convulsion during her sleep. As she lives alone, there is no witness to the event. Her GP assumes that the history indicates both focal seizures and a generalised seizure. Jen is prescribed carbamazepine 200mg twice daily.
Referral and diagnosis
Jen returns four weeks later as she is concerned that her hand twitching has increased. Her GP refers her for a neurological assessment.
The neurologist orders an EEG, which shows a generalised spike wave discharge when Jen is asleep. She also has a photoconvulsive response to flashing lights. The neurologist makes a diagnosis of a genetic generalised epilepsy (juvenile myoclonic epilepsy) based on the history of daytime myoclonic and absence seizures, the nocturnal generalised seizure and the EEG findings. Brain imaging is not recommended.
Management
In juvenile myoclonic epilepsy, carbamazepine is likely to exacerbate the myoclonic seizures. Although sodium valproate is the medication of choice, it has the potential for teratogenic and neurodevelopmental effects on an exposed foetus. The neurologist recommends that Jen starts on levetiracetam. Jen is advised to stop driving because of her daytime absence seizures.
Health Navigator. Search for “epilepsy” at healthify.nz
Epilepsy New Zealand. epilepsy.org.nz
My Medicines. mymedicines.nz
Valproate risk in pregnancy. sanofi.com.au/valproate
ACC. Medicines for epilepsy, mental health, and pain can harm your unborn baby: Talk to your doctor about the risks to you and your baby, and how to balance them. May 2020 – available at acc.co.nz/treatmentsafety
New Zealand Formulary. nzf.org.nz
New Zealand Formulary for Children. nzfchildren.org.nz
Regional HealthPathways. healthify.nz/healthcare-providers/r/regional-healthpathways-links-hcps
International League Against Epilepsy. ilae.org
EpilepsyDiagnosis.org. epilepsydiagnosis.org
Paediatric Neurology Clinical Network. Epilepsy Guidelines and Pathways for Children and Young People. June 2017. https://bit.ly/2ZA5TsD
National Institute for Health and Care Excellence. Epilepsies: diagnosis and management. February 2020. nice.org.uk/guidance/cg137
ACC. Benefits and risks of taking anti-seizure medicines for epilepsy, mental health, or pain: Information for healthcare professionals to discuss with anyone who could get pregnant. May 2020 – available at acc.co.nz/treatmentsafety
Suzanne Davis is a retired paediatric neurologist and president of the New Zealand League Against Epilepsy
Elizabeth Walker is a neurologist and clinical neurophysiologist at Auckland City Hospital, and honorary senior clinical lecturer at the University of Auckland School of Medicine
This 12-question multiple-choice assessment is designed to demonstrate that the provided educational reading has been effective in allowing you to meet the learning objectives of this course. Write down your answers to these questions.
1. Which TWO of the following are included in the International League Against Epilepsy’s definition of epilepsy?
a. at least two unprovoked (or reflex) epileptic seizures occurring less than 24 hours apart
b. at least two unprovoked (or reflex) epileptic seizures occurring more than 24 hours apart
c. one unprovoked (or reflex) epileptic seizure with any probability of experiencing a second seizure
d. one unprovoked (or reflex) epileptic seizure with a moderate to high probability of experiencing a second seizure (>30%)
e. one unprovoked (or reflex) epileptic seizure with a high probability of experiencing a second seizure (>60%)
2. Which TWO of the following terms are no longer used by the International League Against Epilepsy for classification of epileptic seizure types?
a. focal impaired awareness seizure
b. focal to bilateral tonic-clonic seizure
c. generalised tonic-clonic seizure
d. partial complex seizure
e. secondarily generalised seizure
3. Alan visits you after he lost consciousness while shopping earlier that day, while with his partner. She says the 34-year-old had twitching of both legs (and possibly arms) and his head was “hitting the ground”. It all lasted for about 15 seconds, after which he took a minute or two to return to full consciousness. This is the first time this has happened. Which of the following diagnoses is the most likely?
a. absence seizure
b. convulsive syncope
c. generalised tonic-clonic seizure
d. juvenile myoclonic seizure
4. Belinda crashed her car after she lost consciousness on a long drive home one Sunday afternoon after visiting friends. The 19-year-old escaped with minor injuries, passed an alcohol breath test and no one else was hurt. Witnesses state the car left the straight, level highway and slipped into a ditch, having already slowed somewhat. What is the most likely cause of the accident?
a. driver fatigue
b. seizure
5. Which of the following tests used to investigate epileptic disorders is often performed after sleep deprivation to increase the likelihood of finding diagnostic abnormalities?
a. complete blood count
b. CT scan
c. electroencephalogram
d. MRI scan
6. Which of the following anti-seizure medications is the best tolerated first-line choice for focal-onset epilepsy?
a. carbamazepine
b. lamotrigine
c. levetiracetam
d. sodium valproate
7. Holly is a 28-year-old woman who has generalised epilepsy with tonic-clonic seizures. Which TWO of the following anti-seizure medications would be the most appropriate to consider as first-line therapy for her?
a. carbamazepine
b. lamotrigine
c. levetiracetam
d. sodium valproate
8. Holly, the 28-year-old patient with generalised tonic-clonic seizures, is started on lamotrigine. What THREE pieces of advice should she be given regarding contraception and pregnancy?
a. if she plans a pregnancy, she should see a neurologist six to 12 months before discontinuing contraception
b. lamotrigine dose and blood levels must be closely monitored if she becomes pregnant
c. lamotrigine is safe for use during pregnancy, so she does need to worry about using contraception
d. lamotrigine poses a dose-related risk to the foetus, so her dose should be reduced before planning a pregnancy
e. depot medroxyprogesterone acetate injections or an intrauterine device (plus condoms) would be better options than oral contraceptives as they do not affect lamotrigine levels
9. All anti-seizure medications are associated with behavioural side effects. Which TWO of the following drugs have the highest risk of significant psychiatric adverse effects, including depression?
a. carbamazepine
b. lamotrigine
c. levetiracetam
d. sodium valproate
e. topiramate
10. Driving is a difficult aspect of epilepsy management. Chris is 23 years old and has had two seizures this week after being seizure free for three years on medication, which he takes reliably and regularly. He has been under work stress and had poor sleep starting a month ago, but he is now sleeping better. Which TWO options are possible stand-down periods from driving that are applicable to Chris?
a. no stand-down required if a non-recurring cause for his seizures is clearly identified
b. two months if his sleep deprivation has resolved
c. <12 months if a positive neurologist recommendation is obtained
d. 12 months, as laid out in NZ Transport Agency regulations for anyone experiencing a seizure
e. Chris is permanently unfit to drive as he has medication-resistant epilepsy
11. Preventable injuries and deaths during seizures are not uncommon. What is the most common cause of death brought about by seizures?
a. choking
b. drowning
c. head injury
d. traffic accidents
12. Sudden unexpected death in epilepsy is rare, but it is a concern for patients and families. Which THREE of the following are risk factors for SUDEP?
a. male sex
b. nocturnal seizures
c. old age at onset of seizures
d. tonic-clonic seizures
e. treatment with sodium valproate
f. uncontrolled epilepsy
Write down your answers to these questions. Then, to check your answers and record your score, click here.
You can use the Capture button below to record your time spent reading and your answers to the following learning reflection questions, which align with Te Whanake reflection requirements (answer three or more):
- What were the key learnings from this activity?
- How does what you learnt benefit you, or why do you appreciate the learning?
- If you apply your learning, what are the benefits or implications for others?
- Think of a situation where you could apply this learning. What would you do differently now?
- If an opportunity to apply this learning comes up in the future, what measures can be taken to ensure the learning is applied?
- Can you think of any different ways you could apply this learning?
- Are there any skills you need to develop to apply this learning effectively?
We're publishing this article as a FREE READ so it is FREE to read and EASY to share more widely. Please support us and our primary care education resources – subscribe here
- Fisher RS, Cross JH, French JA, et al. Operational classification of seizure types by the International League Against Epilepsy: Position paper of the ILAE Commission for Classification and Terminology. Epilepsia 2017;58(4):522–30.
- Scheffer IE, Berkovic S, Capovilla G, et al. ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58(4):512–21.
- Fiest KM, Sauro KM, Wiebe S, et al. Prevalence and incidence of epilepsy: A systematic review and meta-analysis of international studies. Neurology 2017;88(3):296–303.
- Bergin PS, Brockington A, Jayabal J, et al. Status epilepticusin Auckland, New Zealand: Incidence, etiology, and outcomes. Epilepsia 2019;60(8):1552–64.







![Barbara Fountain, editor of New Zealand Doctor Rata Aotearoa, and Paul Hutchison, GP and senior medical clinician at Tāmaki Health [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/Barbara%20Fountain%2C%20editor%20of%20New%20Zealand%20Doctor%20Rata%20Aotearoa%2C%20and%20Paul%20Hutchison%2C%20GP%20and%20senior%20medical%20clinician%20at%20T%C4%81maki%20Health%20CR%20Simon%20Maude.jpg?itok=-HbQ1EYA)
![Lori Peters, NP and advanced health improvement practitioner at Mahitahi Hauora, and Jasper Nacilla, NP at The Terrace Medical Centre in Wellington [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/2.%20Lori%20Peters%2C%20NP%20and%20advanced%20HIP%20at%20Mahitahi%20Hauora%2C%20and%20Jasper%20Nacilla%2C%20NP%20at%20The%20Terrace%20Medical%20Centre%20in%20Wellington%20CR%20Simon%20Maude.jpg?itok=sUfbsSF1)
![Ministry of Social Development health and disability coordinator Liz Williams, regional health advisors Mary Mojel and Larah Takarangi, and health and disability coordinators Rebecca Staunton and Myint Than Htut [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/3.%20Ministry%20of%20Social%20Development%27s%20Liz%20Williams%2C%20Mary%20Mojel%2C%20Larah%20Takarangi%2C%20Rebecca%20Staunton%20and%20Myint%20Than%20Htut%20CR%20Simon%20Maude.jpg?itok=9ceOujzC)
![Locum GP Helen Fisher, with Te Kuiti Medical Centre NP Bridget Woodney [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/4.%20Locum%20GP%20Helen%20Fisher%2C%20with%20Te%20Kuiti%20Medical%20Centre%20NP%20Bridget%20Woodney%20CR%20Simon%20Maude.jpg?itok=TJeODetm)
![Ruby Faulkner, GPEP2, with David Small, GPEP3 from The Doctors Greenmeadows in Napier [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/5.%20Ruby%20Faulkner%2C%20GPEP2%2C%20with%20David%20Small%2C%20GPEP3%20from%20The%20Doctors%20Greenmeadows%20in%20Napier%20CR%20Simon%20Maude.jpg?itok=B0u4wsIs)
![Rochelle Langton and Libby Thomas, marketing advisors at the Medical Protection Society [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/6.%20Rochelle%20Langton%20and%20Libby%20Thomas%2C%20marketing%20advisors%20at%20the%20Medical%20Protection%20Society%20CR%20Simon%20Maude.jpg?itok=r52_Cf74)
![Specialist GP Lucy Gibberd, medical advisor at MPS, and Zara Bolam, urgent-care specialist at The Nest Health Centre in Inglewood [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/7.%20Specialist%20GP%20Lucy%20Gibberd%2C%20medical%20advisor%20at%20MPS%2C%20and%20Zara%20Bolam%2C%20urgent-care%20specialist%20at%20The%20Nest%20Health%20Centre%20in%20Inglewood%20CR%20Simon%20Maude.jpg?itok=z8eVoBU3)
![Olivia Blackmore and Trudee Sharp, NPs at Gore Health Centre, and Gaylene Hastie, NP at Queenstown Medical Centre [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/8.%20Olivia%20Blackmore%20and%20Trudee%20Sharp%2C%20NPs%20at%20Gore%20Health%20Centre%2C%20and%20Gaylene%20Hastie%2C%20NP%20at%20Queenstown%20Medical%20Centre%20CR%20Simon%20Maude.jpg?itok=Z6u9d0XH)
![Mary Toloa, specialist GP at Porirua and Union Community Health Service in Wellington, Mara Coler, clinical pharmacist at Tū Ora Compass Health, and Bhavna Mistry, specialist GP at Porirua and Union Community Health Service [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/9.%20Mary%20Toloa%2C%20Porirua%20and%20Union%20Community%20Health%20Service%20in%20Wellington%2C%20Mara%20Coler%2C%20T%C5%AB%20Ora%20Compass%20Health%2C%20and%20Bhavna%20Mistry%2C%20PUCHS%20CR%20Simon%20Maude.jpg?itok=kpChr0cc)