Prostate cancer consultations are common in primary care and there is no one approach to testing and treatment that fits all patients. Urologist Simon van Rij discusses the key considerations and options for personalised care, appropriate investigation and treatment
Frequently misunderstood and debilitating condition put under the spotlight
Frequently misunderstood and debilitating condition put under the spotlight
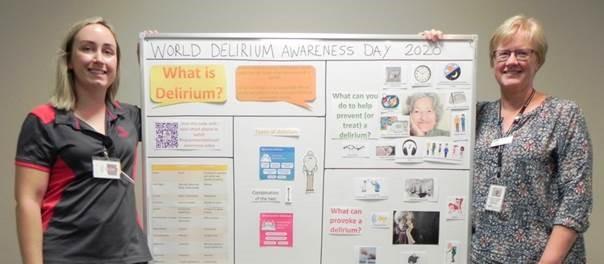
Delirium is a debilitating condition affecting thousands of New Zealanders annually but is often missed and frequently misunderstood says a healthcare expert. But taking some simple measures can help those affected.
“There are things everyone can do to recognise delirium and help those affected,” said Bay of Plenty District Health Board (BOPDHB) Clinical Nurse Specialist - Older Adult - Catherine Mounsey.
“Delirium may be confused with dementia but it is different in that it has a sudden onset and is often reversible, whereas dementia has a gradual onset and becomes progressively worse over time,” added Catherine, ahead of World Delirium Awareness Day, on Wednesday 11 March. “Delirium is more likely to affect older people, those who are physically frail, on multiple medications, experiencing a new illness, or worsening of an existing illness, or those who have had an injury.
“We’re looking to raise awareness about delirium and how people can recognise the signs of it in their loved ones and what they can do to help them.”
So what is delirium?
Delirium is a sudden onset of confusion also known as acute brain failure. It may begin rapidly (hours to minutes) or come on more gradually (days to weeks) and is often the result of illness or injury.
With an older person there can often be multiple causes such as dehydration, constipation, change of environment and many others. A person with delirium has a disturbance in the brain’s function and each person will experience it differently.
These experiences may include:
- Being more confused than normal
- Difficulty maintaining attention or following a conversation
- Difficulty knowing what’s going on around them
- Seeing or hearing things that aren’t there
- Feeling restless or agitated
- Being more sleepy or more awake than normal
How can I help?
Knowing whether the person is different to usual is key, so information from someone who knows them well is very important. Please share this information with healthcare professionals.
Glasses and hearing aids are very important in helping the person with delirium. If a person is in hospital, bring in familiar items from home such as photographs, personal items, calendar or small clock / watch.
You can visit the person regularly but limit the number of visitors as this can overwhelm the person. Identify yourself and address yourself by name “Good morning mum, it’s Susan”.
Use a calm tone and gentle touch to reassure and calm your loved one and try not to argue with unusual thoughts and comments. You may need to orientate them often and let them know why they are here. Mobilising, eating and drinking are important for the person’s recovery and you may be able to assist with this. Please ask hospital staff how you can help.
Often becoming more confused may be the first sign of an older person becoming unwell. If you notice this at home, please seek early assessment from their GP.
How is delirium treated?
Treatment looks at addressing underlying conditions. It is important to find and treat all potential causes. There are also non-pharmacological treatments that are just as important to aid in recovery.
Once the causes of delirium are found and treated, many people make a good recovery, however sometimes older people or those with dementia take longer or may not recover completely.