Respiratory physician Lutz Beckert considers chronic obstructive pulmonary disease management, including the prevention of COPD, the importance of smoking cessation and pulmonary rehabilitation, and the lifesaving potential of addressing treatable traits. He also discusses the logic of inhaler therapy, moving from single therapy to dual and triple therapy when indicated, as well as other aspects of management
HealthPathways: A Canterbury tale From paper tiger in Christchurch to asset in consult rooms globally
HealthPathways: A Canterbury tale From paper tiger in Christchurch to asset in consult rooms globally

Fiona Cassie explores how HealthPathways has grown from helping Canterbury general practices to shedding light on clinical decisionmaking and health resources in many parts of the world
"They were debating whether to put it in a ringbinder or, it was 2007, to get sophisticated and put it on a CD"
It began with a thick wodge of paper sitting on a table.
But, as in all good origin stories, there are slight variations in the telling.
As Ian Anderson recalls it, he came across specialist GP Graham McGeoch wondering how to get that paper wodge, detailing a new respiratory clinical pathway, out to Canterbury general practices.
“They were debating whether to put it in a ringbinder or, it was 2007, to get sophisticated and put it on a CD,” Mr Anderson remembers with a chuckle.
Mr Anderson, as the co-founder of technical writing business Streamliners, suggested they leave it with his team. A week later he returned with the first online HealthPathways prototype.
It offered GPs a web-based, clickable local guideline to assessing, managing and referring patients with chronic obstructive pulmonary disease to Canterbury specialist services.
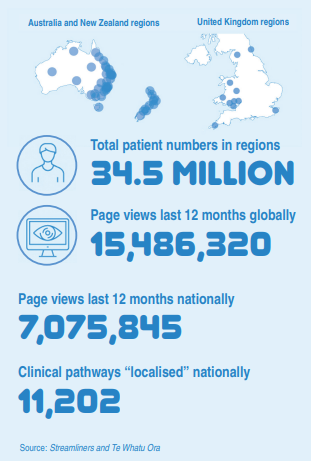
HealthPathways now covers 600- plus clinical conditions and is used by GPs, nurse practitioners, nurses and allied health clinicians across New Zealand, Australia, England and Wales.
The pathways web platform was launched in 2008 as a collaboration between Canterbury DHB, local GPs and Streamliners. When other DHBs started knocking on Canterbury’s doors wanting HealthPathways, they were pointed towards Streamliners for support to localise and implement pathways in their regions.
The Christchurch-based company now provides ongoing pathways management and coordination for the 11 regional groupings that cover the country and another 50 health systems globally. Together they make up the HealthPathways Community collaboration.
Streamliners, meanwhile, has gone from eight staff in 2008 to 150 in 2023 and a $20 million turnover. The company is doubling the size of its Christchurch-based headquarters to support the international growth in HealthPathways.
Dr McGeoch, dubbed the “father of HealthPathways”, says he had no idea back in 2007 it would go global. He just wanted to build a locally consistent clinical guidance manual.
The first pathway, co-written with respiratory physician Roland Meyer with DHB funding, was the typically textheavy guideline you might expect from two slightly academic doctors, he says.
The DHB, then under the leadership of chief executive David Meates and innovative planning and funding manager Carolyn Gullery, was fostering the “high trust, clinician-led, management-supported, whole system” approach to health that Canterbury became famous for after the 2010/11 earthquakes.
Part of that whole-of-system approach is the Canterbury Initiative, a collaboration of GPs and hospital specialists focused on using innovation and integration to improve healthcare.
Dr McGeoch says the initiative was kicked off in 2007 when the DHB funded him and fellow specialist GP and Pegasus Health founder David Kerr to work with project manager Bruce Penny to “sort out the referrals process”.
Mr Anderson, who had been a Canterbury Health planning manager in the 1990s before he founded Streamliners, offered the trio a neutral space to meet: in his company’s building.
And that is how Mr Anderson came upon them debating whether, as Dr McGeoch recalls it, to distribute the COPD pathway as some kind of flipchart, a printed document or maybe the “really modern” CD-ROM. “None of which anybody would have looked at,” agrees Dr McGeoch in retrospect.
Instead, Mr Anderson took the complex document to the “mother of HealthPathways”, Streamliners technical writer Juanita Gibson, to pare it down to key items in a template structure that has stood the test of time.
GPs’ positive feedback to this pilot pathway led to other respiratory pathways being added, along with gynaecological referral guidelines written by specialist GP Clare Healy and gynaecologist Mike East.
Now having critical mass, the project launched the HealthPathways website in 2008. By the end of 2009, 135 pathways offered succinct evidence-based information on assessing and managing patients with everything from headaches to bowel cancer symptoms.
Consistent guidance for specialist referrals was also being negotiated between specialist GPs and hospital specialists and updated regularly to reflect what hospitals could deliver.
At the same time, funding and training to deliver services including spirometry to pipelle biopsies and to access diagnostic testing was being devolved from secondary to primary care to reduce avoidable referrals.
Come 2013 and Canterbury clinicians and Streamliners had developed over 600 HealthPathways being used by nearly all Canterbury GPs along with local variations available across most of New Zealand and in many Australian states.
That same year, HealthPathways was hailed by the UK’s The King’s Fund as being part of the integration-led “transformation” of the Canterbury health system.
The increased international profile and positive research findings on reduced waiting lists and avoidable referrals saw HealthPathways taken up by some NHS regions in the UK. A successful rollout in Cardiff and Vale led to the NHS Wales in April signing up to implement HealthPathways nationally – the first country in the world to do so.
It has been a heady 15 years for Mr Anderson as HealthPathways took Streamliners from a local technical writing start-up to a global player with its Christchurch-based clinical editors and technical team working with 61 regional health systems.
His own induction to the health system came in 1995, during the Crown Health Enterprise days. The commerce graduate, with a background in the manufacturing and electricity sectors, became Canterbury Health planning manager, responsible for Christchurch Hospital.
“I was one of the commercial people brought in to ‘fix’ the health system,” he says.
It took a couple of years for him to realise health didn’t fit the normal business model and “you are in the rationing business”.
And, Mr Anderson says, he found people working in the health system weren’t motivated by commercial drivers but by “delivering really good health and social outcomes for patients”.
He also noted the sector was “a concentration of the brightest people in the country”.
In time, he concluded that what works for the health system is hightrust, effective relationships and getting the right information to front-line people to let them do their job. That was the culture of the much-missed “dream team” of Mr Meates and Ms Gullery, whom Mr Anderson worked with in the 2000s and until their departures in 2020.
But first he had to deal with the damning 1996 Patients are Dying report into Christchurch Hospital patient deaths by senior clinicians, and the follow-up 1998 report by health and disability commissioner Robyn Stent.
“It was a horrible time,” he recalls. “Treasury had a philosophy of setting the board against the management and management against the clinicians. It was a divide and conquer mindset and it was a disaster, in my opinion.”
He left Canterbury Health in 1999, setting up Streamliners with his technical writer wife Emma Harding while continuing some health planning contract work in the company’s early days.
Streamliners launched the policy documentation SchoolDocs platform in 2006 (now a standalone sister company), followed it up with the general practice-focused GPDocs in 2016 and, more recently, the student wellbeing pathway platform Stronger Schools.
But it is HealthPathways and its association with the Canterbury health “transformation” that has led Streamliners’ global expansion. There are more countries on the horizon; Mr Anderson had an early morning online meeting with a Canadian health authority the day of his interview with New Zealand Doctor Rata Aotearoa.
I was one of the commercial people brought in to “fix” the health system
At home in New Zealand, some GPs have had mixed feelings about HealthPathways as it became associated with rationing of scarce secondary health services.
Wellington specialist GP Emma Dunning wrote in 2016 of it sometimes seeming “secondary care is using HealthPathways as a tool against us”.
Last year, Whangārei specialist GP Paula Mathieson talked of HealthPathways becoming a “de facto means to decline referrals”.
The father of HealthPathways is not surprised at the guarded response from some GPs.
“HealthPathways needs to be good, accurate clinical guidance for general practice teams,” Dr McGeoch says. “But it also needs to be a negotiating tool for what the hospital is actually going to do and what public services are going to be available to patients in a transparent and equitable manner.”
Few, if any, regions around the country took Canterbury’s comprehensive approach to HealthPathways as a tool for health improvement and change management.
One result is that the number of generic pathways that have been localised to reflect and respond to the reality of secondary services varies significantly across the 11 HealthPathways regions.
Streamliners data show Canterbury clinicians use of HealthPathways remains two to five-fold higher per capita than most other regions.
Some DHBs “starved” their HealthPathways programmes by not investing the time and money to create localised pathways that were correct and current and had buy-in from secondary clinicians, Mr Anderson says.
“You need trust and agreement between primary and secondary clinicians,” he says. “And it’s hard to get agreement if you don’t have the trust.”
When GPs click on HealthPathways and find them out of date and out of touch with referral realities, their engagement wanes.
RNZCGP medical director Luke Bradford says GPs support and make good use of pathways where they are well established, backed by clinician working groups and reflect local services.
“But I suspect where the mahi behind it and the clear roots aren’t there, then they are just not used…they are seen as just another button to press that doesn’t help,” says Dr Bradford, a Tauranga specialist GP.
Mr Anderson is used to HealthPathways being criticised by some as being a rationing tool.
But he says a good HealthPathways programme just tells the truth and reflects the reality.
“Would they rather it didn’t tell the truth? If [secondary services] are not going to see patients below a certain threshold of need, surely the GP and the patient need to know that?”
The key, he says, is that if patient access to specialist services is restricted, then planners and commissioners have to be upfront and support general practices to keep managing those patients in the community.
“Just hiding the problem is not good for anybody.”
Dr McGeoch says an example in the early days of HealthPathways was the Canterbury Initiative negotiating training and funding for GPs to do routine skin lesion removals in response to a backlog of plastic surgery referrals.
More recently, when Te Whatu Ora Canterbury had no dermatologist for some time, HealthPathways were updated regularly to keep clinicians in the know.
Mr Anderson says doctor shortages, overloaded hospitals and ambulance “ramping” are making headlines in every country where Streamliners is working.
The answer is making better use of primary and community services and that means funding them “properly” to deliver extra services, he says.
“You can’t just keep saying, ‘we’d like general practice to do that or this community service provider to do that’ without remunerating them to do it,” Mr Anderson says.
And he believes HealthPathways – that wodge of paper that grew into a global health tool – can play its part in revealing health system strengths and weaknesses, and finding solutions.
HealthPathways is variously described as an “online manual”, “decision support tool” and “information portal” for general practice teams and other community healthcare providers.
GPs and other clinicians log into their local portal to the HealthPathways website to see what and where will be the next step for their patient.
The pathways cover more than 600 clinical conditions.
Each pathway provides concise guidance on patient assessment, management and referrals to ease discussion during patient consultations.
Localised pathways also include agreed thresholds for specialist referrals in that region and any expanded diagnostic or general practice services supported locally.
HealthPathways started in Canterbury but pathways have been adopted, adapted and shared by 60 other regional health systems around New Zealand and the world.
Christchurch couple Ian Anderson and Emma Harding, whose technical writing company Streamliners became the backbone of HealthPathways, were keen to ensure it wasn’t “gobbled up by a profit-motivated big corporate”.
So, as of 30 June, they transferred 80 per cent of the shares to the Joined Up Systems Trust (JUST), which aims to support integration of health and social services.
The remainder went to the New Zealand Health Innovation Hub (formerly part of Canterbury DHB, now owned by Te Whatu Ora).
The HealthPathways web platform was launched in 2008 as a collaboration between Canterbury DHB, local GPs and Streamliners.
Content for the first pathways was developed by Canterbury DHB and shared for free to other regions of New Zealand. Then, in 2013, HealthPathways was picked up in Australia, with clients paying a licensing fee to Canterbury DHB.
When Australia started localising its own pathways in 2015, the licensing fee was stopped, says Mr Anderson.
Instead, he says, there was a handshake agreement for the DHB to take a 20 per cent stake in Streamliners.
The couple began investigating the idea of a charitable trust. It took until 2022 to establish it and vest the 80 per cent in it, while allocating the balance to the DHB hub.
Under the handshake agreement, profits had been put back into improving HealthPathways for Canterbury and the other 50 health systems that make up the HealthPathways Community.
If any new intellectual property is created by partner health systems, the agreement is the property belongs to its creator but is licensed so Streamliners can distribute it to other community members.
HealthPathways has been used to help reveal the “postcode lottery” differences in healthcare access across the Tasman and similar work is planned here.
Ian Anderson, chief executive of HealthPathways’ co-developer Streamliners, says the pathways can make transparent the inconsistencies faced by general practices in accessing secondary services for their patients across the country.
The key to using HealthPathways to reveal the postcode lottery is for all local pathways to stick to being true and upfront about the reality of services available, Mr Anderson says.
In Australia, Streamliners worked with Queensland Health to modify regional HealthPathways to reflect new statewide access criteria to secondary hospital and diagnostic services.
Streamliners insisted that, in regions where patient services available to general practices didn’t match what the state says should be available, actual local circumstances were clearly stated.
Then local differences recorded in HealthPathways were used by Queensland Health to identify regions where it needed to work on resolving access issues, says Mr Anderson.
Streamliners and Te Whatu Ora recently signed a letter of intent to replace the current 11 HealthPathways agreements with a single national agreement covering New Zealand.
Te Whatu Ora national director improvements and innovation Dale Bramley says the move will include developing priority national pathways and using these to highlight unwarranted variation in access to patient services across regions.
The first national pathways were developed and continually updated in response to the COVID-19 pandemic.
When the Delta strain hit in August 2021, Mr Anderson says, Streamliners worked urgently with the Ministry of Health to develop a pathway to help practices manage COVID-19 in the community.
The resulting COVID-19 management pathway is the country’s most popular pathway, with nearly 240,000 clinician views in 12 months, followed by the COVID-19 antivirals pathway with about 85,000 views.
Tonsillitis, hypertension and headaches in adults were also among the most-viewed pathways in the year to January.
The regions with the most localised pathways are Canterbury, the West Coast and Nelson-Marlborough, followed by the Auckland, Southern and lower North Island regions.







![Barbara Fountain, editor of New Zealand Doctor Rata Aotearoa, and Paul Hutchison, GP and senior medical clinician at Tāmaki Health [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/Barbara%20Fountain%2C%20editor%20of%20New%20Zealand%20Doctor%20Rata%20Aotearoa%2C%20and%20Paul%20Hutchison%2C%20GP%20and%20senior%20medical%20clinician%20at%20T%C4%81maki%20Health%20CR%20Simon%20Maude.jpg?itok=-HbQ1EYA)
![Lori Peters, NP and advanced health improvement practitioner at Mahitahi Hauora, and Jasper Nacilla, NP at The Terrace Medical Centre in Wellington [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/2.%20Lori%20Peters%2C%20NP%20and%20advanced%20HIP%20at%20Mahitahi%20Hauora%2C%20and%20Jasper%20Nacilla%2C%20NP%20at%20The%20Terrace%20Medical%20Centre%20in%20Wellington%20CR%20Simon%20Maude.jpg?itok=sUfbsSF1)
![Ministry of Social Development health and disability coordinator Liz Williams, regional health advisors Mary Mojel and Larah Takarangi, and health and disability coordinators Rebecca Staunton and Myint Than Htut [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/3.%20Ministry%20of%20Social%20Development%27s%20Liz%20Williams%2C%20Mary%20Mojel%2C%20Larah%20Takarangi%2C%20Rebecca%20Staunton%20and%20Myint%20Than%20Htut%20CR%20Simon%20Maude.jpg?itok=9ceOujzC)
![Locum GP Helen Fisher, with Te Kuiti Medical Centre NP Bridget Woodney [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/4.%20Locum%20GP%20Helen%20Fisher%2C%20with%20Te%20Kuiti%20Medical%20Centre%20NP%20Bridget%20Woodney%20CR%20Simon%20Maude.jpg?itok=TJeODetm)
![Ruby Faulkner, GPEP2, with David Small, GPEP3 from The Doctors Greenmeadows in Napier [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/5.%20Ruby%20Faulkner%2C%20GPEP2%2C%20with%20David%20Small%2C%20GPEP3%20from%20The%20Doctors%20Greenmeadows%20in%20Napier%20CR%20Simon%20Maude.jpg?itok=B0u4wsIs)
![Rochelle Langton and Libby Thomas, marketing advisors at the Medical Protection Society [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/6.%20Rochelle%20Langton%20and%20Libby%20Thomas%2C%20marketing%20advisors%20at%20the%20Medical%20Protection%20Society%20CR%20Simon%20Maude.jpg?itok=r52_Cf74)
![Specialist GP Lucy Gibberd, medical advisor at MPS, and Zara Bolam, urgent-care specialist at The Nest Health Centre in Inglewood [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/7.%20Specialist%20GP%20Lucy%20Gibberd%2C%20medical%20advisor%20at%20MPS%2C%20and%20Zara%20Bolam%2C%20urgent-care%20specialist%20at%20The%20Nest%20Health%20Centre%20in%20Inglewood%20CR%20Simon%20Maude.jpg?itok=z8eVoBU3)
![Olivia Blackmore and Trudee Sharp, NPs at Gore Health Centre, and Gaylene Hastie, NP at Queenstown Medical Centre [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/8.%20Olivia%20Blackmore%20and%20Trudee%20Sharp%2C%20NPs%20at%20Gore%20Health%20Centre%2C%20and%20Gaylene%20Hastie%2C%20NP%20at%20Queenstown%20Medical%20Centre%20CR%20Simon%20Maude.jpg?itok=Z6u9d0XH)
![Mary Toloa, specialist GP at Porirua and Union Community Health Service in Wellington, Mara Coler, clinical pharmacist at Tū Ora Compass Health, and Bhavna Mistry, specialist GP at Porirua and Union Community Health Service [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/9.%20Mary%20Toloa%2C%20Porirua%20and%20Union%20Community%20Health%20Service%20in%20Wellington%2C%20Mara%20Coler%2C%20T%C5%AB%20Ora%20Compass%20Health%2C%20and%20Bhavna%20Mistry%2C%20PUCHS%20CR%20Simon%20Maude.jpg?itok=kpChr0cc)