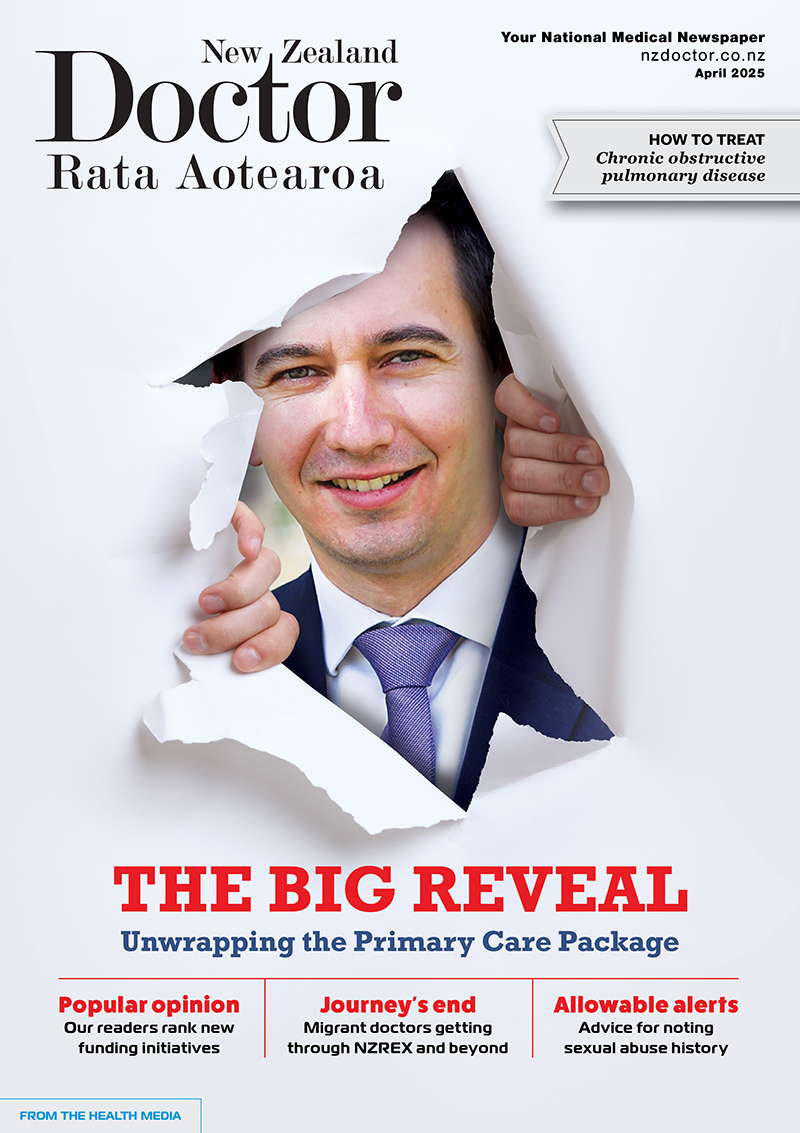
Respiratory physician Lutz Beckert considers chronic obstructive pulmonary disease management, including the prevention of COPD, the importance of smoking cessation and pulmonary rehabilitation, and the lifesaving potential of addressing treatable traits. He also discusses the logic of inhaler therapy, moving from single therapy to dual and triple therapy when indicated, as well as other aspects of management
Ten-year HIV elimination plan fails to recognise impact on wāhine Māori
Ten-year HIV elimination plan fails to recognise impact on wāhine Māori
Public health researcher Clive Aspin has welcomed the Government’s 10-year HIV elimination plan but says it does not reflect HIV’s disproportionate impact on wāhine Māori.
Failure to recognise the elevated risk for Māori, and especially Māori women, is a “glaring omission” that could easily derail the plan’s goals and worsen inequities, says Dr Aspin (Ngāti Maru, Ngāti Whanaunga, Ngāti Tamaterā).
The poukairangi Māori/associate dean Māori and senior lecturer in health at Victoria University, he says the HIV pandemic is changing, with groups besides gay and bisexual men now at risk.
Māori women comprise 20 per cent of cases among women infected in Aotearoa while Māori as a whole make up 15 per cent of the population, he points out.
The impact of the plan, which has $18 million over four years from Budget 2022, will be limited unless Māori women are considered an at-risk group, especially as they are more likely to be diagnosed late, Dr Aspin says.
The Government paid “scant attention” to a 1994 Ministry of Māori Development report on the likely impact of HIV on Māori.
Three community consultations on the current draft have been set for Auckland, Wellington and Christchurch this month and, while Dr Aspin is pleased the LGBTQ+ community is being consulted, he says the Government must also get feedback from other affected communities. Health officials need to broaden their perspective, he says, and be ready to act even if the feedback doesn’t fit their expectations.
New Zealand Sexual Health Society sexual health physician Massimo Giola says physicians mostly only test patients for HIV if they fit the stereotype of “the promiscuous, gay man”.
The LGBTQ+ community, gay and bisexual men are also more confident in getting tested, says Dr Giola: “The gay community has a long history of resilience, agency, positive and proactive health-seeking behaviour.”
Dr Aspin says practitioners need to address their “blind spot”, as women living with HIV are experiencing delays in diagnosis because they are not seen as at-risk. He says HIV funding historically goes to male-dominated community organisations, but the money and resources for eliminating HIV should now be distributed equally among affected communities.
At the Burnett Foundation Aotearoa (formerly New Zealand AIDS Foundation), chief executive Joe Rich says his group has been serving the LGBTQ+ community for over 40 years.
Positive Women, a support organisation for women and families living with and affected by HIV, is great for people who don’t feel represented by other services, Mr Rich says.
In a press release, associate health minister Ayesha Verrall says one of the plan’s goals is to “improve Māori health and wellbeing in relation to HIV”.
The plan proposes greater access to sexual health services, greater responsiveness for HIV in primary care, and more at-home testing options. Action is to focus on: surveillance, information and knowledge systems; prevention and health promotion; testing and linkage to care; and support for people living with HIV.
We're publishing this article as a FREE READ so it is FREE to read and EASY to share more widely. Please support us and the hard work of our journalists by clicking here and subscribing to our publication and website



![Barbara Fountain, editor of New Zealand Doctor Rata Aotearoa, and Paul Hutchison, GP and senior medical clinician at Tāmaki Health [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/Barbara%20Fountain%2C%20editor%20of%20New%20Zealand%20Doctor%20Rata%20Aotearoa%2C%20and%20Paul%20Hutchison%2C%20GP%20and%20senior%20medical%20clinician%20at%20T%C4%81maki%20Health%20CR%20Simon%20Maude.jpg?itok=-HbQ1EYA)
![Lori Peters, NP and advanced health improvement practitioner at Mahitahi Hauora, and Jasper Nacilla, NP at The Terrace Medical Centre in Wellington [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/2.%20Lori%20Peters%2C%20NP%20and%20advanced%20HIP%20at%20Mahitahi%20Hauora%2C%20and%20Jasper%20Nacilla%2C%20NP%20at%20The%20Terrace%20Medical%20Centre%20in%20Wellington%20CR%20Simon%20Maude.jpg?itok=sUfbsSF1)
![Ministry of Social Development health and disability coordinator Liz Williams, regional health advisors Mary Mojel and Larah Takarangi, and health and disability coordinators Rebecca Staunton and Myint Than Htut [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/3.%20Ministry%20of%20Social%20Development%27s%20Liz%20Williams%2C%20Mary%20Mojel%2C%20Larah%20Takarangi%2C%20Rebecca%20Staunton%20and%20Myint%20Than%20Htut%20CR%20Simon%20Maude.jpg?itok=9ceOujzC)
![Locum GP Helen Fisher, with Te Kuiti Medical Centre NP Bridget Woodney [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/4.%20Locum%20GP%20Helen%20Fisher%2C%20with%20Te%20Kuiti%20Medical%20Centre%20NP%20Bridget%20Woodney%20CR%20Simon%20Maude.jpg?itok=TJeODetm)
![Ruby Faulkner, GPEP2, with David Small, GPEP3 from The Doctors Greenmeadows in Napier [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/5.%20Ruby%20Faulkner%2C%20GPEP2%2C%20with%20David%20Small%2C%20GPEP3%20from%20The%20Doctors%20Greenmeadows%20in%20Napier%20CR%20Simon%20Maude.jpg?itok=B0u4wsIs)
![Rochelle Langton and Libby Thomas, marketing advisors at the Medical Protection Society [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/6.%20Rochelle%20Langton%20and%20Libby%20Thomas%2C%20marketing%20advisors%20at%20the%20Medical%20Protection%20Society%20CR%20Simon%20Maude.jpg?itok=r52_Cf74)
![Specialist GP Lucy Gibberd, medical advisor at MPS, and Zara Bolam, urgent-care specialist at The Nest Health Centre in Inglewood [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/7.%20Specialist%20GP%20Lucy%20Gibberd%2C%20medical%20advisor%20at%20MPS%2C%20and%20Zara%20Bolam%2C%20urgent-care%20specialist%20at%20The%20Nest%20Health%20Centre%20in%20Inglewood%20CR%20Simon%20Maude.jpg?itok=z8eVoBU3)
![Olivia Blackmore and Trudee Sharp, NPs at Gore Health Centre, and Gaylene Hastie, NP at Queenstown Medical Centre [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/8.%20Olivia%20Blackmore%20and%20Trudee%20Sharp%2C%20NPs%20at%20Gore%20Health%20Centre%2C%20and%20Gaylene%20Hastie%2C%20NP%20at%20Queenstown%20Medical%20Centre%20CR%20Simon%20Maude.jpg?itok=Z6u9d0XH)
![Mary Toloa, specialist GP at Porirua and Union Community Health Service in Wellington, Mara Coler, clinical pharmacist at Tū Ora Compass Health, and Bhavna Mistry, specialist GP at Porirua and Union Community Health Service [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/9.%20Mary%20Toloa%2C%20Porirua%20and%20Union%20Community%20Health%20Service%20in%20Wellington%2C%20Mara%20Coler%2C%20T%C5%AB%20Ora%20Compass%20Health%2C%20and%20Bhavna%20Mistry%2C%20PUCHS%20CR%20Simon%20Maude.jpg?itok=kpChr0cc)