Respiratory physician Lutz Beckert considers chronic obstructive pulmonary disease management, including the prevention of COPD, the importance of smoking cessation and pulmonary rehabilitation, and the lifesaving potential of addressing treatable traits. He also discusses the logic of inhaler therapy, moving from single therapy to dual and triple therapy when indicated, as well as other aspects of management
GPs burning out, working one day a week for free
GPs burning out, working one day a week for free

We can’t blame it all on COVID…before the pandemic hit, things were hard
The average GP is working nearly one day a week for free and is at a growing risk of burnout, the RNZCGP’s latest workforce survey shows.
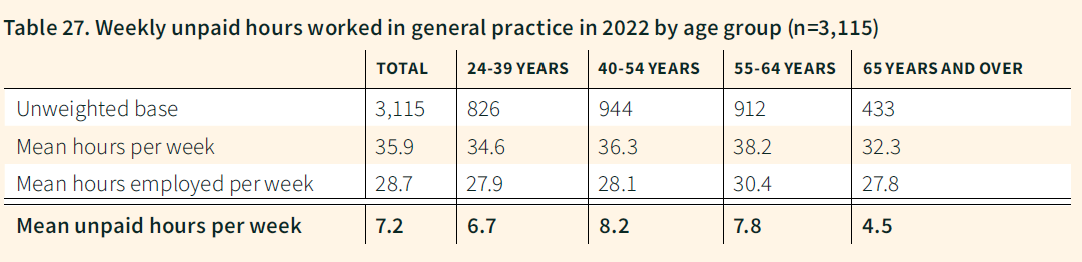
The 2022 General Practice Workforce Survey reveals GPs on average are employed for 28.7 hours of the 35.9 hours they work, meaning the average GP is not paid for 7.2 hours a week.
“That is effectively almost a day of work they are doing that is not remunerated,” says college president and specialist GP Samantha Murton.
“Every one of us is doing extra work out of hours, on the weekend or during our lunch break...well, we don’t have lunch breaks,” Dr Murton says.
The 2022 survey – carried out last winter during the Omicron outbreak – was the first time the survey asked GPs how many hours they work as well as how many hours they are employed.
GPs’ total hours worked per week were up from 34.8 hours in 2020 and 2018 and were the highest since 2014.
Dr Murton says most of the additional hours are due to GP shortages, but disease complexity and delays to secondary care also play a part.
She says the problem is, GP remuneration is linked to seeing patients. The solution is reforming the out-of-date general practice funding model, which is no longer “fit for purpose”.
The percentage of GPs intending to retire in the next five years rose to 37 per cent, up from 31 per cent in the last survey in 2020.
The 2022 survey was released this morning as Dr Murton prepared to present the findings to health minister Ayesha Verrall, and to call for solutions such as training more medical students and higher remuneration for specialist GPs.
Dr Murton tells New Zealand Doctor Rata Aotearoa she is heartened by the response rate: 72 per cent of college members. That’s a record rate since the voluntary survey began in 2014.
She says the nearly 3300 GP responses are “awesome” as they give the college a clear mandate when seeking solutions to GP shortages and burnout.
The response rate also reflects GPs’ readiness to “tell it like it is”, their commitment to the sector and the need for better working conditions, says Dr Murton.
In the latest survey, 48 per cent of GPs rate themselves as burned out – that is, scoring between 7 and 10 on a scale ranging from 0 (not at all) to 10 (extreme). The proportion is up on 2020’s 31 per cent and more than double 2016’s 22 per cent.
When GPs who are “somewhat” burned out (score 4 to 6) are included, 79 per cent of GP respondents report some level of burnout.
Dr Murton says COVID-19 has been “extraordinarily difficult”, but adds: “We can’t blame it all on COVID…before the pandemic hit, things were hard.
“And even if we hadn’t had COVID, I believe burnout would be genuinely increasing.”
The proportion of GPs likely to recommend general practice as a career fell from 54 per cent in 2020 to 39 per cent in the latest survey. Thirty per cent are neutral and 31 per cent report they are unlikely to recommend a general practice career.
READ MORE FROM THE 2020 WORKFORCE SURVEY:
- THE MISSING - It’s no myth: making sense of the RNZCGP 2020 workforce survey
- THE PAY GAP: Huge gender pay gap confronts general practice workforce
- THE RURALS: Rural healthcare: Where the rubber hits the road with GP shortage
- THE DIVERSITY: It's a waiting game before GPs truly represent the country they serve
Thirty per cent of GPs are now aged 60 or older and 37 per cent of GPs responding to the survey want to retire in the next five years.
About 425 specialist GPs aged over 65 are still practising. which Dr Murton says on the positive side shows the “real joy they have in their job and they don’t want to stop”.
But she says the college estimates that, if those GPs (14 per cent of the workforce) retired immediately, it would lead to about 725,000 more New Zealanders being without a doctor.
The largest proportion of the GP workforce (36 per cent) is aged 24 to 44. Only 33 per cent are 45 to 59 years: Dr Murton says this “missing middle” is due to a decision made in the 1990s to train far fewer GPs.
Dr Murton says one answer to GP workforce issues is to “massively up the number of medical school graduates”.
She points to Ireland, with a similar population to New Zealand, where 750 locals and 750 international students graduate as doctors each year.
“Their universities are churning them out, so let’s start churning,” says Dr Murton.
She says medical training and the health system also need to recognise and value the general practice specialist service provided by fellows of the college.
“[Fellowship] equals zero dollars for graduates,” she says. For example, ACC recognises and pays different rates to rural health medicine and urgent care fellows, but not to general practice fellows.
“The invidious position we are in is that our job is challenging but fantastic, really rewarding, makes a difference to people’s lives and is very gratifying.
“It’s great job but the working conditions and financial rewards need to be just as great and currently they are not.”
-
Median GP age remains at 52 and the average age is 50.6.
-
Female GPs make up 58 per cent of the workforce, male 42 per cent and gender diverse/not specified 1 per cent (rounding means total is more than 100 per cent)
-
Ethnicity: European 69 per cent, Asian 20 per cent, Māori 5 per cent, Middle Eastern, Latin American or African 3 per cent, Pacific 2 per cent, other 2 per cent.
-
$166,389 was the average all GP personal, before-tax income ($157,594 in 2020). The median was $137,500.
-
$212,500 ($200,000 in 2020) was the male median income for full-time GPs compared with the female median income of $162,500 ($160,000 in 2020).
For full coverage of the RNZCGP 2022 survey, see our next issue, out on April 12.
We're publishing this article as a FREE READ so it is Free to read and Easy to share more widely. Please support our journalism and coverage of issues that matter to primary care – subscribe here









![Barbara Fountain, editor of New Zealand Doctor Rata Aotearoa, and Paul Hutchison, GP and senior medical clinician at Tāmaki Health [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/Barbara%20Fountain%2C%20editor%20of%20New%20Zealand%20Doctor%20Rata%20Aotearoa%2C%20and%20Paul%20Hutchison%2C%20GP%20and%20senior%20medical%20clinician%20at%20T%C4%81maki%20Health%20CR%20Simon%20Maude.jpg?itok=-HbQ1EYA)
![Lori Peters, NP and advanced health improvement practitioner at Mahitahi Hauora, and Jasper Nacilla, NP at The Terrace Medical Centre in Wellington [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/2.%20Lori%20Peters%2C%20NP%20and%20advanced%20HIP%20at%20Mahitahi%20Hauora%2C%20and%20Jasper%20Nacilla%2C%20NP%20at%20The%20Terrace%20Medical%20Centre%20in%20Wellington%20CR%20Simon%20Maude.jpg?itok=sUfbsSF1)
![Ministry of Social Development health and disability coordinator Liz Williams, regional health advisors Mary Mojel and Larah Takarangi, and health and disability coordinators Rebecca Staunton and Myint Than Htut [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/3.%20Ministry%20of%20Social%20Development%27s%20Liz%20Williams%2C%20Mary%20Mojel%2C%20Larah%20Takarangi%2C%20Rebecca%20Staunton%20and%20Myint%20Than%20Htut%20CR%20Simon%20Maude.jpg?itok=9ceOujzC)
![Locum GP Helen Fisher, with Te Kuiti Medical Centre NP Bridget Woodney [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/4.%20Locum%20GP%20Helen%20Fisher%2C%20with%20Te%20Kuiti%20Medical%20Centre%20NP%20Bridget%20Woodney%20CR%20Simon%20Maude.jpg?itok=TJeODetm)
![Ruby Faulkner, GPEP2, with David Small, GPEP3 from The Doctors Greenmeadows in Napier [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/5.%20Ruby%20Faulkner%2C%20GPEP2%2C%20with%20David%20Small%2C%20GPEP3%20from%20The%20Doctors%20Greenmeadows%20in%20Napier%20CR%20Simon%20Maude.jpg?itok=B0u4wsIs)
![Rochelle Langton and Libby Thomas, marketing advisors at the Medical Protection Society [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/6.%20Rochelle%20Langton%20and%20Libby%20Thomas%2C%20marketing%20advisors%20at%20the%20Medical%20Protection%20Society%20CR%20Simon%20Maude.jpg?itok=r52_Cf74)
![Specialist GP Lucy Gibberd, medical advisor at MPS, and Zara Bolam, urgent-care specialist at The Nest Health Centre in Inglewood [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/7.%20Specialist%20GP%20Lucy%20Gibberd%2C%20medical%20advisor%20at%20MPS%2C%20and%20Zara%20Bolam%2C%20urgent-care%20specialist%20at%20The%20Nest%20Health%20Centre%20in%20Inglewood%20CR%20Simon%20Maude.jpg?itok=z8eVoBU3)
![Olivia Blackmore and Trudee Sharp, NPs at Gore Health Centre, and Gaylene Hastie, NP at Queenstown Medical Centre [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/8.%20Olivia%20Blackmore%20and%20Trudee%20Sharp%2C%20NPs%20at%20Gore%20Health%20Centre%2C%20and%20Gaylene%20Hastie%2C%20NP%20at%20Queenstown%20Medical%20Centre%20CR%20Simon%20Maude.jpg?itok=Z6u9d0XH)
![Mary Toloa, specialist GP at Porirua and Union Community Health Service in Wellington, Mara Coler, clinical pharmacist at Tū Ora Compass Health, and Bhavna Mistry, specialist GP at Porirua and Union Community Health Service [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/9.%20Mary%20Toloa%2C%20Porirua%20and%20Union%20Community%20Health%20Service%20in%20Wellington%2C%20Mara%20Coler%2C%20T%C5%AB%20Ora%20Compass%20Health%2C%20and%20Bhavna%20Mistry%2C%20PUCHS%20CR%20Simon%20Maude.jpg?itok=kpChr0cc)