Otolaryngologist, head and neck surgeon Francis T. Hall discusses the evaluation of thyroid nodules, which primarily aims to determine the likelihood of malignancy. He then reviews the treatment of thyroid nodules and thyroid cancer, including recent advances in management
Eye problems give clues to systemic impact of COVID-19
Eye problems give clues to systemic impact of COVID-19
The ocular complications of COVID-19 are varied and can serve as important indicators of disease severity. This article explains why recognising these manifestations is essential
- Follicular conjunctivitis can be an early sign and prognostic factor for COVID-19.
- Retinal vein occlusion associated with COVID-19 is a marker for a systemic prothrombotic response.
- COVID-19 is associated with sight and life-threatening conditions, and may lead to chronic ocular issues, including dry eye and neuro-ocular symptoms similar to those observed in concussion.
- Early detection and appropriate referral is crucial in mitigating long-term vision loss and improving patient outcomes.
This Practice article has been endorsed by the RNZCGP and has been approved for up to 0.5 credits for continuing professional development purposes (2 credits per learning hour). To claim your CPD credits, log in to your Te Whanake dashboard and record this activity under the appropriate learning category.
Nurses may also find that reading this article and reflecting on their learning can count as a professional development activity with the Nursing Council of New Zealand (up to 0.25 PD hours).
The COVID-19 pandemic has profoundly impacted global health, with millions of cases and significant mortality worldwide. The SARS-CoV-2 virus is now becoming endemic, presenting ongoing challenges for healthcare providers.
While the respiratory and neurological complications of COVID-19 are well recognised, the virus can affect multiple organ systems, including the eyes. Approximately 11 per cent of patients with COVID-19 may experience eye symptoms, ranging from conjunctivitis to vision-threatening ocular disease.1 These ocular complications can occur alongside typical COVID-19 symptoms or may present atypically in individuals who are asymptomatic or paucisymptomatic.
Our team has recently completed a comprehensive review of the ocular sequelae associated with COVID-19 (pubmed.ncbi.nlm.nih.gov/38925508).1 In this article, we summarise the key findings, shedding light on the various ways in which COVID-19 can impact ocular health and highlighting the importance of awareness and early detection in managing these complications.
Follicular conjunctivitis is seen in 3 to 13.6 per cent of all patients with COVID-19 and may be the first sign of illness. The conjunctiva is vulnerable to SARS-CoV-2 infection by direct inoculation or spread from the nasolacrimal duct or lacrimal gland. Conjunctival tissue destruction causes release of virus particles into tears, which can be detected in tear PCR testing in a small proportion of patients.1–5
Therefore, it is important to ask patients presenting with a pink eye about exposure to COVID-19, test for COVID-19, and don personal protective equipment (including eye protection) during examination.
COVID-19 follicular conjunctivitis is usually self-limiting and can be treated with cool compresses and artificial tears. However, complications requiring ophthalmology referral can occur. These include pseudomembranous conjunctivitis, conjunctival scarring, corneal pseudodendrites and superimposed bacterial keratitis.2–6 Checking visual acuity, examining the lids for pseudomembranes, and assessing the corneal surface with fluorescein will identify these patients.
The presence of conjunctivitis is also associated with the severity of systemic COVID-19 illness. Patients requiring hospital admission for acute respiratory distress syndrome are at least three times more likely to have a positive conjunctival COVID-19 swab than those with less severe respiratory disease.3,5 Conjunctivitis in a patient with COVID-19 should alert the GP that this patient may have, or may develop, severe disease. They should be monitored regularly for clinical deterioration requiring hospital admission.
It is well established that COVID-19 results in a proinflammatory, prothrombotic immune response which may predispose patients to systemic thromboembolic events up to two years after initial infection. This can occur in patients even with mild COVID-19 respiratory symptoms.
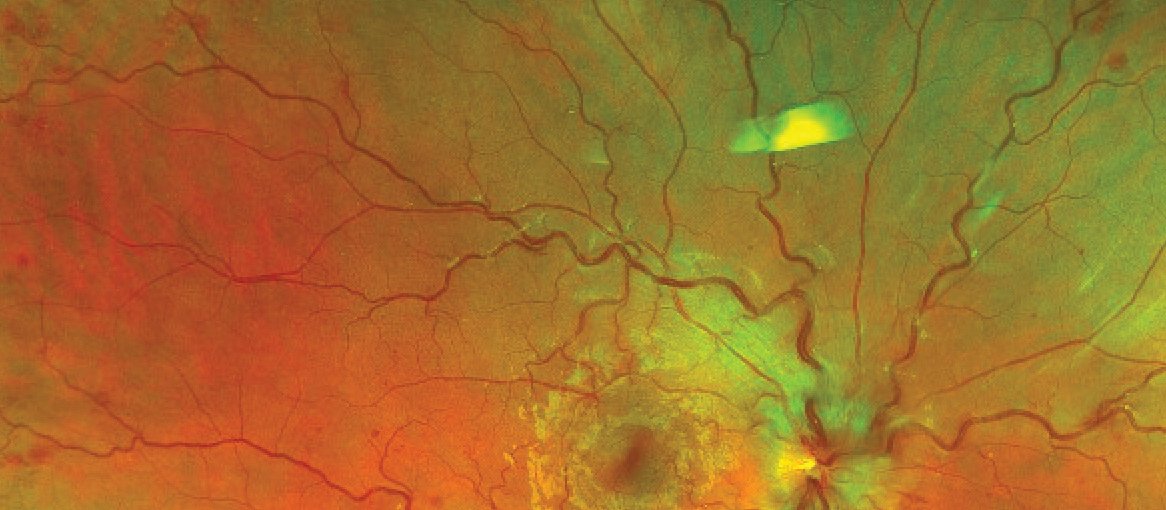
The eyes’ vasculature is vulnerable to injury in such a proinflammatory state. A large retrospective study of 1.4 million US patients demonstrated a twofold increase in branch retinal vein occlusion and 1.5-fold increase in central retinal vein occlusion within 12 weeks of COVID-19 diagnosis. The increased risk of branch retinal vein occlusion extended to two years after COVID-19 diagnosis.7
While retinal vein occlusions usually occur in older people with cardiovascular risk factors, vein occlusions related to COVID-19 tend to occur in young, healthy adults.1
Sudden painless loss of vision in a young person with a white eye, in the context of recent COVID-19, should prompt the GP to think about retinal vein occlusion and perform fundoscopy (Figure 1). If a retinal vein occlusion is diagnosed, we recommend screening for, and managing, the risks of other thrombotic diseases, including stroke, pulmonary embolism and coronary artery disease.
Dysregulated immune function and increased autoimmunity after COVID-19 may predispose patients to uveitis. The risk of a new diagnosis of uveitis is increased by 18 per cent in adults aged 18 to 65 between one month and two years after COVID-19. Most of these patients have a lack of other risk factors for uveitis and a negative uveitis workup.1
Flares of pre-existing uveitis may also occur following COVID-19, requiring a temporary up-titration or change of immunosuppressive therapy.1
In adults, COVID-19 has been associated with rare forms of uveitis, including Vogt–Koyanagi–Harada disease, multiple evanescent white dot syndrome (Figure 2) and acute macular neuroretinopathy.1 New visual symptoms, including blurred vision, photophobia, and shimmering or paracentral scotomas, in a patient with a recent diagnosis of COVID-19, should warrant referral to ophthalmology.
Other unusual ocular presentations of COVID-19 reported in the literature include adult-onset Kawasaki disease with lid swelling, erythema multiforme and conjunctival ulceration.1 Consider testing for COVID-19 in young patients with unusual eye presentations, even in the absence of respiratory symptoms.
Children are at risk of paediatric inflammatory multisystem syndrome (PIMS) and tubulointerstitial nephritis with uveitis (TINU) weeks after COVID-19 due to an excessive inflammatory response to the virus.1,8 PIMS causes widespread rash, conjunctivitis, uveitis, fever, shock and end organ damage. It requires hospital admission for intravenous steroid and/or immunoglobulin.8 TINU is a rare inflammatory disease characterised by bilateral anterior uveitis, acute nephritis and fevers, which requires renal biopsy for diagnosis and immunosuppressive therapy.9
Any child who presents with a red eye, reduced vision and photophobia within weeks of COVID-19 should have their vital signs checked and a thorough skin, cardiovascular and gastrointestinal examination performed, looking for fever, signs of shock and rash. A renal function test should be considered if clinical examination is suggestive of TINU. A suspicion of either PIMS or TINU requires immediate paediatric, nephrology and ophthalmology review for diagnosis and treatment.
GPs are typically the first point of contact for patients with COVID-19; therefore, it is important to be able to identify other sight or life-threatening conditions that present with ocular signs during and after COVID-19.
Endogenous endophthalmitis has been reported in multiple case reports of patients with, or recently recovered from, COVID-19 who have at least one of the following significant risk factors:1
- hospitalisation or intensive care unit admission for severe COVID-19
- intravenous steroid treatment
- type 2 diabetes.
Steroid treatment predisposes patients to opportunistic infections, including Candida albicans and Aspergillus fumigatus. The presence of fungi or yeast endophthalmitis is higher in COVID-related endophthalmitis than non-COVID endophthalmitis and has a poor prognosis.1 Endophthalmitis should be considered in patients with COVID-19 with the aforementioned risk factors who present with decreased acuity, floaters, ocular pain and hypopyon (Figure 3).
Rhino-orbital mucormycosis is another rare opportunistic fungal infection that can affect from 0.08 to 0.7 per cent of patients with current or recent COVID-19. This fungal infection spreads from the sinuses and orbit to surrounding tissues, including the brain, and has a mortality rate of 24 per cent. Risk factors include diabetes and either oral or intravenous steroid use for COVID-19. Patients usually present with proptosis, vision reduced to light perception, and eye pain.1 They require urgent surgical attention.
One in five patients with neurocognitive deficits of long COVID have visual symptoms
Chronic sequelae of COVID-19, or long COVID, affects approximately 10 per cent of all people with COVID-19 worldwide. The main symptoms of long COVID include fatigue, dyspnoea, neurocognitive effects and brain fog.
Interestingly, one in five patients with neurocognitive deficits of long COVID have visual symptoms. These symptoms include reduced visual acuity or change in refractive error, photosensitivity, convergence insufficiency and visual disturbances.1
Some studies have suggested that COVID-19 can also lead to chronic meibomian gland dysfunction, increased severity of dry eye, and chronic neuropathic pain described as “burning eye syndrome”.1 Awareness of these symptoms is important so these concerns are taken seriously and appropriate referrals can be made.
Jahnvee Solanki is a non-vocational ophthalmology registrar working at Greenlane Clinical Centre this year. Rachael Niederer is an ophthalmologist and uveitis and medical retina specialist at Auckland Eye and Greenlane Clinical Centre, and a senior lecturer at the University of Auckland
You can use the Capture button below to record your time spent reading and your answers to the following learning reflection questions, which align with Te Whanake reflection requirements (answer three or more):
- What were the key learnings from this activity?
- How does what you learnt benefit you, or why do you appreciate the learning?
- If you apply your learning, what are the benefits or implications for others?
- Think of a situation where you could apply this learning. What would you do differently now?
- If an opportunity to apply this learning comes up in the future, what measures can be taken to ensure the learning is applied?
- Can you think of any different ways you could apply this learning?
- Are there any skills you need to develop to apply this learning effectively?
We're publishing this article as a FREE READ so it is FREE to read and EASY to share more widely. Please support us and our primary care education resources – subscribe here
1. Ng HW, Scott DAR, Danesh-Meyer HV, et al. Ocular manifestations of COVID-19. Prog Retin Eye Res 2024; 24 June online.
2. Cheema M, Aghazadeh H, Nazarali S, et al. Keratoconjunctivitis as the initial medical presentation of the novel coronavirus disease 2019 (COVID-19). Can J Ophthalmol 2020;55(4):e125–29.
3. Savastano MC, Gambini G, Savastano A, et al. Evidence-based of conjunctival COVID-19 positivity: An Italian experience: Gemelli Against COVID Group. Eur J Ophthalmol 2021;31(6):2886–93.
4. Xia J, Tong J, Liu M, et al. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol 2020;92(6):589–94.
5. Loffredo L, Pacella F, Pacella E, et al. Conjunctivitis and COVID-19: A meta-analysis. J Med Virol 2020;92(9):1413–14.
6. Navel V, Chiambaretta F, Dutheil F. Haemorrhagic conjunctivitis with pseudomembranous related to SARS-CoV-2. Am J Ophthalmol Case Rep 2020;19:100735.
7. Li JX, Wei JC, Wang YH, et al. Retinal vascular occlusion and COVID-19 diagnosis: A multicenter population-based study. Retina 2024;44(2):345–52.
8. Singh-Grewal D, Lucas R, McCarthy K, et al. Update on the COVID-19-associated inflammatory syndrome in children and adolescents; paediatric inflammatory multisystem syndrome-temporally associated with SARS-CoV-2. J Paediatr Child Health 2020;56(8):1173–77.
9. Janetos TM, Lee PHA, Goldstein DA. Tubulointerstitial nephritis and uveitis syndrome in pediatric patients. Ocul Immunol Inflamm 2023;31(10):1955–64.








![New Zealand Doctor Rata Aotearoa editor Barbara Fountain, RNZCGP president elect and Tauranga-based specialist GP Luke Bradford, Ministry of Health clinical chief advisor rural health Helen MacGregor, and Health New Zealand Te Whatu Ora clinical director primary and community care Sarah Clarke [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/1.%20Barbara%20Fountain%2C%20Luke%20Bradford%2C%20Helen%20MacGregor%20and%20Sarah%20Clarke.jpg?itok=091NETXI)
![Ngāti Porou Oranga specialist GP Elina Pekansaari and Te Nikau Hospital specialist in general practice and rural hospital medicine David Short [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/2.%20Elina%20Pekansaari%20and%20David%20Short.jpg?itok=h5XfSBVM)
![Locum specialist GP Margriet Dijkstra and OmniHealth regional operations manager (southern) Patricia Morais-Ross [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/3.%20Margriet%20Dijkstra%20and%20Patricia%20Morais-Ross.jpg?itok=jkrtRfJC)
![Golden Bay dairy farmer and dairy industry health and safety doctoral student Deborah Rhodes, and Golden Bay Community Health specialist GP Rachael Cowie [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/4.%20Deborah%20Rhodes%20and%20Rachael%20Cowie.jpg?itok=oM0_GcJc)
![Hauora Taiwhenua clinical director rural health Jeremy Webber, Australian College of Rural and Remote Medicine president Rod Martin and Observa Care director of business operations Deborah Martin, the wife of Dr Martin [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/5.%20Jeremy%20Webber%2C%20Rod%20Martin%20and%20Deborah%20Martin%2C%20the%20wife%20of%20Dr%20Martin.jpg?itok=P_aGmX_H)
![Spark Health chief executive John Macaskill-Smith and client director Bryan Bunz [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/6.%20John%20Macaskill-Smith%20and%20Bryan%20Bunz.jpg?itok=5yJvVZ0I)
![Associate dean (rural) Kyle Eggleton, third-year medical student Roselle Winter, and second-year pharmacy student Alina Khanal, all from the University of Auckland [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/7.%20Kyle%20Eggleton%2C%20Roselle%20Winter%20and%20Alina%20Khanal.jpg?itok=RQLd3TEs)
![Health New Zealand Te Whatu Ora clinical editor and specialist in general practice and rural hospital medicine Anu Shinnamon, and Whakarongorau chief clinical officer Ruth Large [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/8.%20Anu%20Shinnamon%20and%20Ruth%20Large.jpg?itok=i5TMswY9)
![Te Kahu Hauora Practice specialist GP Jane Laver and Ngāti Kahungunu ki Tāmaki-nui-a-Rua chief operations manager Tania Chamberlain [Image: NZD]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-05/9.%20Jane%20Laver%20and%20Tania%20Chamberlain.jpg?itok=jtMklaCZ)