Otolaryngologist, head and neck surgeon Francis T. Hall discusses the evaluation of thyroid nodules, which primarily aims to determine the likelihood of malignancy. He then reviews the treatment of thyroid nodules and thyroid cancer, including recent advances in management
Evidence-based app teaches young people skills to improve wellbeing
Evidence-based app teaches young people skills to improve wellbeing
Child psychiatrist and paediatrician Hiran Thabrew discusses how mental health and wellbeing apps can help young people learn emotional self-regulation skills
This Practice article has been endorsed by the RNZCGP and has been approved for up to 0.25 credits for continuing professional development purposes (1 credit per learning hour). To claim your CPD credits, log in to your Te Whanake dashboard and record this activity under the appropriate learning category.
Nurses may also find that reading this article and reflecting on their learning can count as a professional development activity with the Nursing Council of New Zealand (up to 0.25 PD hours).
Maia is a 13-year-old ākonga (student) who has been experiencing worries about her studies and how to “fit in” since moving to high school. She has also begun to cut herself when she feels lower in mood. Her mother brings her into your clinic to get some help.
Josh is a 16-year-old apprentice mechanic who has been experiencing anger outbursts over the past few months. Home life has been stressful since his parents split up, and his girlfriend recently said she wants to go out with someone else. He attends your clinic with a black eye following an altercation with a classmate.
Kupe is an 18-year-old tangata taiohi (young man) who is referred to the university counselling service by his tutor after he begins to experience panic attacks around the time of exams. On review, he reveals that he has been comfort eating and binge drinking to manage his feelings.
All three young people have difficulties with emotional self-regulation that are leading to problems with behaviour, anxiety and/or low mood. Self-regulation is defined as the ability to control one’s behaviour, emotions and thoughts in the pursuit of long-term goals.1
Skills for emotional self-regulation (also known as “coping skills”) are essential for wellbeing and are usually learnt during childhood and early adulthood through modelling and experience. Such coping skills may broadly be categorised as functional or healthy in nature when they relieve stress and help to manage situations, and dysfunctional or unhealthy when they lead to personal or external harm.
During adolescence, young people experience numerous developmental and environmental challenges. Given their increased cognitive abilities (especially development of abstract thinking), they may begin to utilise more sophisticated skills for emotional self-regulation. They are also at risk of learning unhealthy ways to manage stress that continue to be used throughout adulthood (eg, using substances, self-harm and acting out).
While there are many ways to help young people learn skills for emotional self-regulation, we know from clinical experience and research that there are no universally preferred strategies and that, in essence, different things work for different people.
Traditionally, many self-regulation strategies were embedded within face-to-face talking therapies (psychotherapies). For instance, problem solving and goal setting were part of cognitive therapies; deep breathing and progressive muscle relaxation were part of behaviour therapies; and sensory focus exercises were part of mindfulness-based therapies.
As our understanding of the overlap between different mental health problems has improved, we have learnt that the acquisition of self-regulation skills can have transdiagnostic benefits.2 Such skills can be learnt either in an individual or combined manner.
Yes. Given their increasing health literacy and their preference for trying self-help over external mental health support in the first instance, young people are more actively learning ways to manage their wellbeing these days.
Further, given their status as “digital natives”, high rates of smartphone access (including among rangatahi Māori3) and difficulties accessing stretched face-to-face services, many young people are open to learning self-regulation skills via technology.4
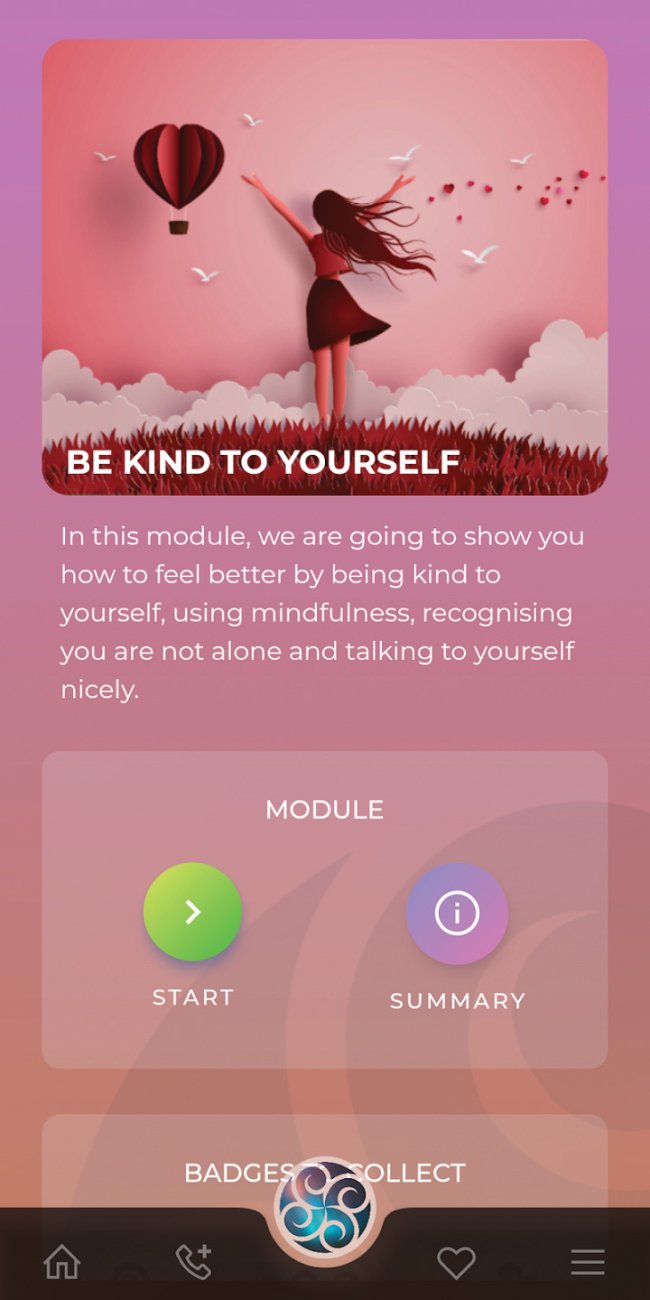
Whitu – 7 Ways in 7 Days is a wellbeing app that was co-designed and developed by young people, Māori, Pacific and digital mental health researchers at the University of Auckland. As its name suggests, it includes seven modules based on principles of positive psychology, cognitive behavioural therapy and psychoeducation that can be completed within a week (see panel). The app opens with a karanga (Māori welcome song) and has consciously been designed to be culturally appealing to Māori and Pacific young people.5
Users are encouraged to trial a range of strategies, discover new ones, and keep using the ones that work best for them. Badge rewards and daily notifications encourage app completion and reuse. Data entered by users are stored in an unencrypted database on their device and can be safely removed at any time by deleting the app.
Whitu is free to use and can be downloaded from the App Store (tinyurl.com/Whitu-Apple) and Google Play (tinyurl.com/Whitu-Google).
Module 1: Feel
Introduces the concept of identifying and monitoring emotions, and identifying adaptive and maladaptive coping skills.
Module 2: Relax
Introduces relaxation techniques, such as deep breathing, progressive muscle relaxation and guided visualisation.
Module 3: Be kind to yourself
Introduces the concept of self-compassion, and users are guided through a short meditation and self-kindness writing exercise.
Module 4: Be thankful
Introduces the concept of gratitude and how it is linked to positive wellbeing.
Module 5: Connect
Users are encouraged to identify important people in their lives and practise ways of staying connected with them.
Module 6: Look after your body
Users are encouraged to eat more healthily, identify and use available forms of exercise, and practise good sleep hygiene.
Module 7: Set goals
Users are introduced to SMART goals and encouraged to practise setting and achieving at least one such goal.
To date, three clinical trials have been conducted with positive results. In 2020, an open trial of Whitu demonstrated improvements in wellbeing, anxiety and depression among young people aged 16 and over, as well as the feasibility of a larger trial.6
In 2021, a subsequent randomised controlled trial with the same age group demonstrated similarly impressive benefits in emotional wellbeing (p=0.005), mental wellbeing (p=0.027), self-compassion (p<0.001), sleep (p=0.018), stress (p=0.002) and depression (p=0.030), with effects sustained at three-month follow-up. Levels of anxiety also reduced to a non-significant degree at four weeks, and to a significant degree (p=0.042) at three months. The app was culturally acceptable to Māori users.7
A more recent RCT with university students also found improvements in wellbeing (p=0.005), mental wellbeing (p=0.027), self-compassion (p=0.001), stress (p=0.002), sleep (p=0.018) and depression (p=0.030; results being prepared for publication).
There have not been any reported adverse effects from using Whitu during these three clinical trials.
No. While there are over 20,000 health apps currently available worldwide, the majority are not evidence based, nor are they culturally relevant for young people in Aotearoa. For more information about those that do meet these criteria, check out the Healthify He Puna Waiora website (healthify.nz/apps; previously Health Navigator).
Whitu may be a useful first-line intervention for young people who either present with self-regulation problems or who are incidentally identified as such. It can be a useful option to “put on the table”, along with speaking to a health improvement practitioner (HIP), primary service psychologist or specialist mental health clinician.
Medication is usually reserved as a second-line intervention or when symptoms are severe and significantly affecting social or occupational functioning.
Just because we are digital immigrants does not mean we cannot learn about new technology
It is best to have read a little about, and ideally tried using, the app. It can be helpful to think about the type and amount of information you would usually provide someone regarding a new medication. Young people need to know what the app does, how long it takes to complete, what it might do to help them and if there are any known adverse effects.
Although many mental health and wellbeing apps are designed as self-help tools, it may also be useful to offer young people some active support (eg, parent supervision) or passive support (eg, a follow-up appointment to see how they fared) to increase app engagement and/or completion.
While it can be easier to avoid discussing health apps due to lack of clinician confidence about technology, remember it’s fine – just because we are digital immigrants does not mean we cannot learn about new technology. We just need to invest a little time to get to know what’s available and how it works. Even spending 15 minutes checking out an app can increase your confidence about prescribing one to your next patient. Healthify provides additional guidance on how to choose a suitable app (tinyurl.com/choosing-apps).
Whitu has recently been adapted for use in high schools, and the new bilingual (English and te reo Māori) version is due to be clinically trialled this year. If the trial results are positive, Whitu for Schools may be a useful, cost-effective and easily disseminable means of teaching high-school students self-regulation-related wellbeing skills before they develop mental health problems. It may also hopefully help to prevent their onset. Watch this space!
Hiran Thabrew is a paediatrician and child psychiatrist at Starship Children’s Hospital, and director of Te Ara Hāro, Centre for Infant, Child and Adolescent Mental Health, University of Auckland
You can use the Capture button below to record your time spent reading and your answers to the following learning reflection questions, which align with Te Whanake reflection requirements (answer three or more):
- What were the key learnings from this activity?
- How does what you learnt benefit you, or why do you appreciate the learning?
- If you apply your learning, what are the benefits or implications for others?
- Think of a situation where you could apply this learning. What would you do differently now?
- If an opportunity to apply this learning comes up in the future, what measures can be taken to ensure the learning is applied?
- Can you think of any different ways you could apply this learning?
- Are there any skills you need to develop to apply this learning effectively?
We're publishing this article as a FREE READ so it is FREE to read and EASY to share more widely. Please support us and our primary care education resources – subscribe here
1. Hofmann W, Schmeichel BJ, Baddeley AD. Executive functions and self-regulation. Trends Cogn Sci 2012;16(3):174–80.
2. Dalgleish T, Black M, Johnston D, Bevan A. Transdiagnostic approaches to mental health problems: Current status and future directions. J Consult Clin Psychol 2020;88(3):179–95.
3. Pacheco E, Melhuish N. Exploring New Zealand children’s internet access, skills and opportunities. Netsafe, September 2019.
4. Thabrew H, Gega L. Editorial: Control alt delete - technology and children's mental health. Child Adolesc Ment Health 2023;28(1):1–3.
5. Serlachius A, Schache K, Boggiss A, et al. Coping skills mobile app to support the emotional well-being of young people during the COVID-19 pandemic: Protocol for a mixed methods study. JMIR Res Protoc 2020;9(10):e23716.
6. Serlachius A, Boggiss A, Lim D, et al. Pilot study of a well-being app to support New Zealand young people during the COVID-19 pandemic. Internet Interv 2021;26:100464.
7. Thabrew H, Boggiss AL, Lim D, et al. Well-being app to support young people during the COVID-19 pandemic: randomised controlled trial. BMJ Open 2022;12(5):e058144.




![Barbara Fountain, editor of New Zealand Doctor Rata Aotearoa, and Paul Hutchison, GP and senior medical clinician at Tāmaki Health [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/Barbara%20Fountain%2C%20editor%20of%20New%20Zealand%20Doctor%20Rata%20Aotearoa%2C%20and%20Paul%20Hutchison%2C%20GP%20and%20senior%20medical%20clinician%20at%20T%C4%81maki%20Health%20CR%20Simon%20Maude.jpg?itok=-HbQ1EYA)
![Lori Peters, NP and advanced health improvement practitioner at Mahitahi Hauora, and Jasper Nacilla, NP at The Terrace Medical Centre in Wellington [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/2.%20Lori%20Peters%2C%20NP%20and%20advanced%20HIP%20at%20Mahitahi%20Hauora%2C%20and%20Jasper%20Nacilla%2C%20NP%20at%20The%20Terrace%20Medical%20Centre%20in%20Wellington%20CR%20Simon%20Maude.jpg?itok=sUfbsSF1)
![Ministry of Social Development health and disability coordinator Liz Williams, regional health advisors Mary Mojel and Larah Takarangi, and health and disability coordinators Rebecca Staunton and Myint Than Htut [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/3.%20Ministry%20of%20Social%20Development%27s%20Liz%20Williams%2C%20Mary%20Mojel%2C%20Larah%20Takarangi%2C%20Rebecca%20Staunton%20and%20Myint%20Than%20Htut%20CR%20Simon%20Maude.jpg?itok=9ceOujzC)
![Locum GP Helen Fisher, with Te Kuiti Medical Centre NP Bridget Woodney [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/4.%20Locum%20GP%20Helen%20Fisher%2C%20with%20Te%20Kuiti%20Medical%20Centre%20NP%20Bridget%20Woodney%20CR%20Simon%20Maude.jpg?itok=TJeODetm)
![Ruby Faulkner, GPEP2, with David Small, GPEP3 from The Doctors Greenmeadows in Napier [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/5.%20Ruby%20Faulkner%2C%20GPEP2%2C%20with%20David%20Small%2C%20GPEP3%20from%20The%20Doctors%20Greenmeadows%20in%20Napier%20CR%20Simon%20Maude.jpg?itok=B0u4wsIs)
![Rochelle Langton and Libby Thomas, marketing advisors at the Medical Protection Society [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/6.%20Rochelle%20Langton%20and%20Libby%20Thomas%2C%20marketing%20advisors%20at%20the%20Medical%20Protection%20Society%20CR%20Simon%20Maude.jpg?itok=r52_Cf74)
![Specialist GP Lucy Gibberd, medical advisor at MPS, and Zara Bolam, urgent-care specialist at The Nest Health Centre in Inglewood [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/7.%20Specialist%20GP%20Lucy%20Gibberd%2C%20medical%20advisor%20at%20MPS%2C%20and%20Zara%20Bolam%2C%20urgent-care%20specialist%20at%20The%20Nest%20Health%20Centre%20in%20Inglewood%20CR%20Simon%20Maude.jpg?itok=z8eVoBU3)
![Olivia Blackmore and Trudee Sharp, NPs at Gore Health Centre, and Gaylene Hastie, NP at Queenstown Medical Centre [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/8.%20Olivia%20Blackmore%20and%20Trudee%20Sharp%2C%20NPs%20at%20Gore%20Health%20Centre%2C%20and%20Gaylene%20Hastie%2C%20NP%20at%20Queenstown%20Medical%20Centre%20CR%20Simon%20Maude.jpg?itok=Z6u9d0XH)
![Mary Toloa, specialist GP at Porirua and Union Community Health Service in Wellington, Mara Coler, clinical pharmacist at Tū Ora Compass Health, and Bhavna Mistry, specialist GP at Porirua and Union Community Health Service [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/9.%20Mary%20Toloa%2C%20Porirua%20and%20Union%20Community%20Health%20Service%20in%20Wellington%2C%20Mara%20Coler%2C%20T%C5%AB%20Ora%20Compass%20Health%2C%20and%20Bhavna%20Mistry%2C%20PUCHS%20CR%20Simon%20Maude.jpg?itok=kpChr0cc)