Respiratory physician Lutz Beckert considers chronic obstructive pulmonary disease management, including the prevention of COPD, the importance of smoking cessation and pulmonary rehabilitation, and the lifesaving potential of addressing treatable traits. He also discusses the logic of inhaler therapy, moving from single therapy to dual and triple therapy when indicated, as well as other aspects of management
Paediatric visual impairment
Paediatric visual impairment
Preventing visual impairment in children is a priority due to the high emotional, social and economic cost for the individual and the wider community. This article, written by Samantha Simkin and Mo Ziaei, highlights the main causes of paediatric visual impairment in Aotearoa New Zealand and the important role GPs play in their early detection. It also covers the key treatments and support services available
This continuing medical education activity has been endorsed by the RNZCGP and has been approved for up to 1 CME credit for continuing professional development purposes (1 credit per learning hour). To claim your credits, log in to your RNZCGP dashboard to record this activity in the CME component of your CPD programme.
Nurses may also find that reading this article and reflecting on their learning can count as a professional development activity with the Nursing Council of New Zealand (up to 1 PD hours).
At the end of this course, you should be able to:
- Recognise common causes of paediatric visual impairment
- Describe the examination of a child with a vision concern
- Identify where to refer a child with reduced vision for treatment and support
This How to Treat assists with the development of the following domains of competence in the general practice curriculum:
- Domain 1: Communication
- Domain 2: Clinical expertise
- Domain 4: Scholarship
- Domain 5: Context of general practice
The aetiology of paediatric visual impairment is diverse and complicated. However, many underlying conditions are preventable or treatable if detected early enough, and some have systemic associations that should be managed urgently.
For cases where vision cannot be saved or improved, establishment and maintenance of key support services is essential for ensuring appropriate development and lifelong success.
Reduced vision at school entry is associated with lower literacy outcomes, with a significant reduction in literary score occurring for each line reduction of visual acuity. Uncorrected visual impairment is also associated with reduced quality of life scores and has significant financial impacts for not only the child but the entire whānau. Therefore, either correction of reduced vision or appropriate support is necessary from a young age.
GPs have a vital role to play in identifying mild to severe reduced vision in children. Key tests should include the red reflex test, visual acuity measurement using a Snellen or logMAR vision chart, ophthalmoscope examination and astute observation of visual behaviour.
In a clinical setting, one should have a low threshold for referral of paediatric ocular conditions for further detailed examination.
GPs are often the first port of call for families with concerns about their child’s vision and can link the family to the appropriate health or support networks to best benefit them. The GP can provide appropriate referral for refractive correction, treatment, management and support.
A significant proportion of children have a vision-affecting condition, particularly myopia and other refractive errors, and having local connections allows you to better support these patients. We encourage you to reach out to your local ophthalmologist (ranzco.edu), optometrists (nzao.nz) or vision support services. For children with lifelong vision problems, particularly those with systemic associations, their GP is the vital link between all their health and support specialists.
The critical period for vision begins at birth and continues up to the age of seven or eight years. The visual input a child receives during this period can have a lifelong impact. Therefore, keen awareness for abnormal or impaired vision in this age group not only changes the child’s present interaction with the world, but their future as well.
In older children, the importance of appropriately managed vision cannot be understated. Education, both formal and informal, relies heavily on vision. Therefore, correction of vision, where possible, or educational support is required for affected children to minimise the impact on their education, productivity and potential.
Children with reduced vision do not necessarily comment on their symptoms as they often do not know what “normal” vision is. Thus, a lack of visual symptoms does not indicate a lack of visual problems in children. Screening, Well Child assessments and questioning at GP visits can often be the first place a visual problem is detected. You have the power to start the cascade that supports a child to see the world clearly.
This section covers the main causes of paediatric visual impairment in Aotearoa New Zealand, including myopia and other refractive errors.
Congenital cataract
Congenital/paediatric cataract is an opacification of the crystalline lens from birth or developing in childhood. It is still a significant cause of visual impairment, despite improved detection and treatment, affecting approximately one to four in 10,000 children in developed nations.1–4 The majority of congenital cataracts in developed nations are idiopathic, but they can also be caused by hereditary diseases, metabolic disorders and trauma.5
Timely surgical intervention and appropriate optical correction of the surgically induced aphakia (eye without a lens) are essential to prevent permanent, irreversible vision loss due to dense amblyopia (decreased vision due to abnormal visual development; covered in more detail later in this section).5,6
Bilateral cases (Figure 1) should receive surgery between six and eight weeks of age, while unilateral cataracts (Figure 2) are typically removed before six weeks of age due to their higher propensity to cause amblyopia.7,8
Paediatric cataract surgical outcomes have significantly improved due to modern surgical techniques, optimised lens implants, prompt detection and subsequent specialised management.1,5 Optical correction is essential after cataract surgery, and often amblyopia treatment is required due to the strong amblyogenic nature of cataracts.
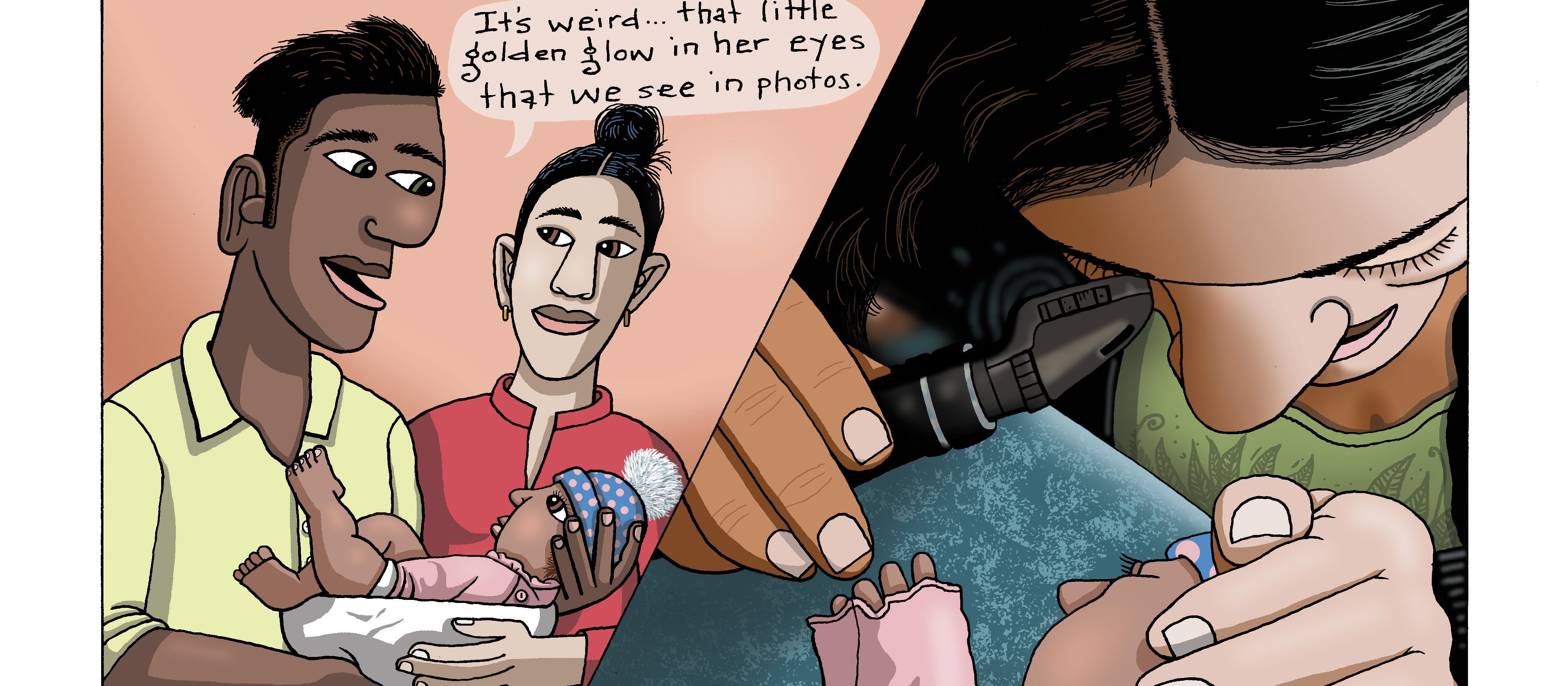
Retinoblastoma
Retinoblastoma is the most common malignant ocular tumour occurring in childhood, with an incidence of approximately one in 18,000 live births. It initiates in embryonic retinal cells and normally occurs before the age of four.9
Common signs of retinoblastoma are an abnormal red reflex or parents describing a “golden glow” in the pupil, either at night-time, when the pupil is dilated or with flash photography.
With early diagnosis and modern therapies, these ocular tumours can be very successfully treated and have survival rates of more than 95 per cent.10 However, in cases where retinoblastoma is detected late or not at all, mortality rates can be as high as 70 per cent, indicating early detection is essential to save lives.9
Cerebral visual impairment
Cerebral visual impairment (CVI), previously known as cortical blindness or cortical visual impairment, is the leading cause of preventable childhood bilateral blindness or low vision in the developed world.11
In New Zealand, the prevalence of CVI is estimated to be 0.02 per cent for children aged 16 and under, making up 30 per cent of all childhood blindness.12
CVI is defined as a bilateral loss of vision with normal ocular structure on ophthalmic examination. It is caused by central nervous system damage to the visual system posterior to the chiasm. However, concurrent anterior visual system disorders can occur. CVI can range in severity from mild visual impairment to blindness.
CVI has a number of underlying aetiologies, with up to 50 per cent of cases having an avoidable cause. New Zealand data published by Chong and Dai in 2014 suggest the division of causes of CVI to be idiopathic (36 per cent), hypoxic (18 per cent) and non-accidental (8 per cent) injury, periventricular leukomalacia, neonatal infections and prematurity.12
Clinical assessment of children with CVI can be extremely challenging due to their complex medical history and often associated global developmental delay. Long-term visual outcomes of CVI are poor, though they can be variable, with current literature stating a possible limited improvement in visual acuity with age.
To date, there is no effective treatment for CVI, so prevention is of paramount significance to reduce the burden of visual impairment associated with it.
Optic nerve hypoplasia
Optic nerve hypoplasia (ONH) is a rare congenital condition when the optic nerve does not fully develop. It is ranked as the fourth most common cause of visual impairment in New Zealand children overall, and as the third most common cause of visual impairment in Māori.13
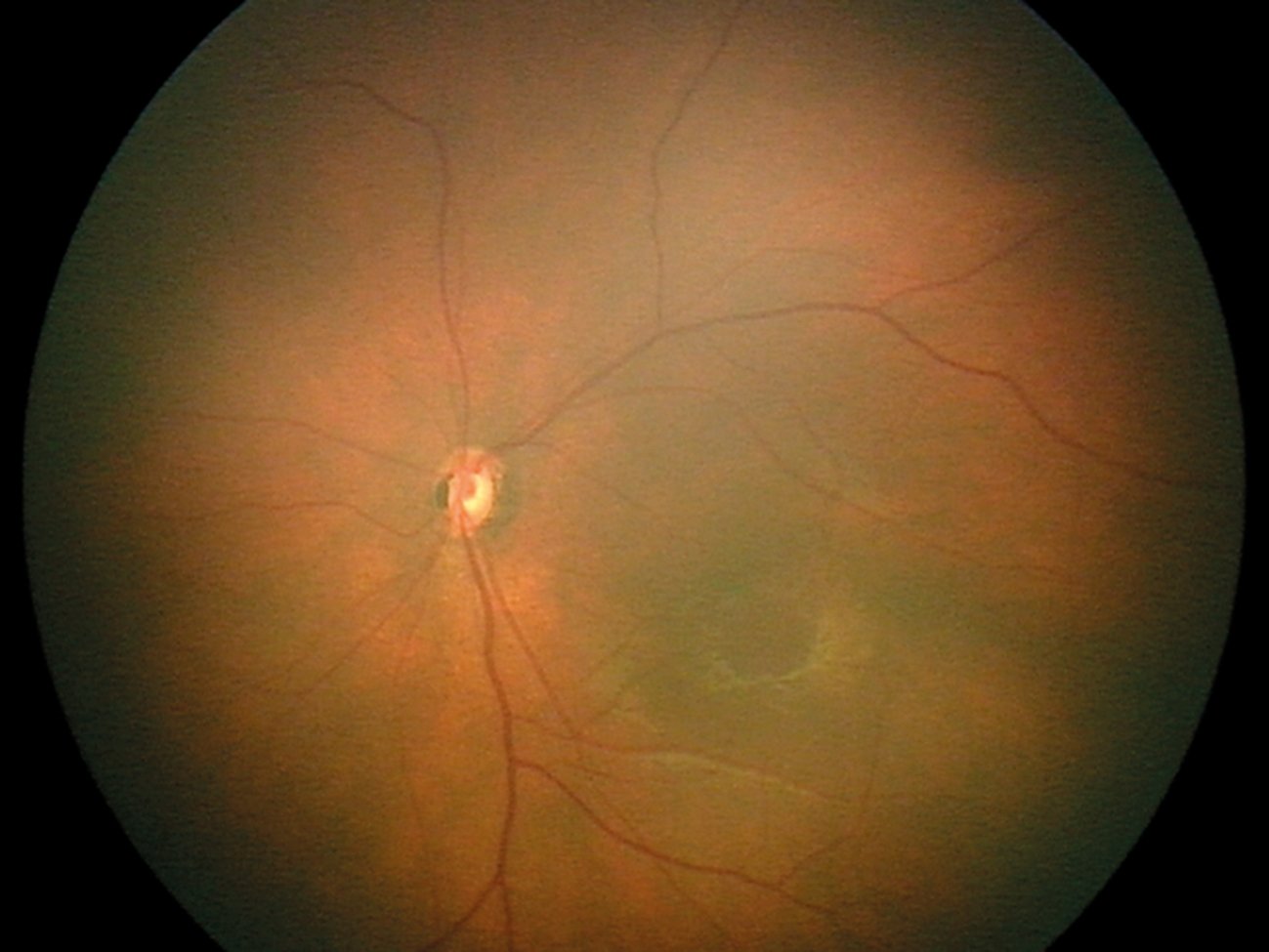
ONH appears as a small and sometimes pale optic nerve, often inside a ring of hypopigmentation known as the “double-ring sign” (Figure 3). The cause of ONH is unknown, although it is associated with young primiparous mothers.
ONH presents with reduced vision from mild visual impairment to complete blindness. Nystagmus – a rhythmic oscillation of the eyes – is often present but may be absent in unilateral cases. While ONH can be detected in isolation, it is commonly associated with cerebral midline structure abnormalities and pituitary axis hormone deficiencies.14 This combination of findings is known as septo-optic dysplasia, and developmental delay and growth restriction can occur in affected children.
There is currently no ophthalmic treatment for optic nerve hypoplasia; however, early detection and management of any associated systemic abnormalities are essential to prevent growth and developmental delay.13
Albinism
Albinism describes a heterogenous group of genetic abnormalities which result in abnormal melanin synthesis and transportation. Phenotypically, albinism presents as a lack of pigmentation. It is not associated with systemic or intellectual abnormalities.
Albinism can be categorised into two main groups: oculocutaneous albinism and ocular albinism, based on involvement of the hair, skin and eyes or the eyes alone, respectively. The prevalence of all types of albinism is approximately one in 17,000 people. The most visible and common type of albinism is oculocutaneous albinism, which comprises 90 per cent of albinism cases. It has an autosomal recessive inheritance pattern.15
Insufficient melanin results in the abnormal development of some ocular structures. Common ocular findings of albinism include reduced visual acuity, nystagmus, iris transillumination (Figure 4) and foveal hypoplasia.16
Visual acuity in individuals with albinism ranges from 6/12 to 6/120.15 The reduction in vision is primarily caused by an absence of the foveal pit – the fovea is normally responsible for our clear central vision.
Vision is further impaired by photophobia and glare as a result of iris transillumination, and retinal light scatter due to a lack of pigment in the eye. Transillumination of the iris is best viewed in a very dark room with a small, bright slit lamp or direct ophthalmoscope beam aimed through the pupil, revealing the retroillumination of the iris.
Cosmetic contact lenses can be used to reduce the effects of glare in older children.
Amblyopia
Amblyopia is a reduction of the best-corrected visual acuity that cannot be attributed to a structural abnormality in the eye. It develops due to an interruption in the normal development of the visual pathway and can be unilateral or bilateral. The prevalence of amblyopia in New Zealand is estimated to be between 1.8 and 3.5 per cent.17
Causes of amblyopia are split into refractive error, strabismus (misalignment of the eyes) and deprivation. Deprivation includes anything that obscures the visual pathway during the critical period of visual development, such as congenital cataract or a droopy lid (ptosis).
Treatment of amblyopia is most effective during the critical period of development, thought to be before the age of eight. This involves eliminating the cause by surgical intervention, glasses correction or other means, and encouraging the use of the visual pathway. In unilateral cases, this often requires patching of the unaffected eye. Bilateral amblyopia has known quality of life impacts, as for any other
bilateral visual impairment. However, more research is needed on the lifelong impacts of unilateral amblyopia. With unilateral amblyopia, there are reports of reduced fine and gross motor development, reduced reading speeds and overall lower academic standing, although this impact is low at a group level in population studies.18
Myopia
Myopia is the most prevalent eye disorder, with projections that over 50 per cent of the population will have myopia by the year 2050.19 It is often downplayed as only a refractive error due to the ability to correct symptoms via glasses, contact lenses or laser refractive surgery.
However, high myopia is linked to increased risk of visual impairment, with myopia over 5 dioptres (pathologic myopia) presenting an increased risk of retinal detachment, myopic maculopathy, myopic choroidal neovascularisation, glaucoma and cataract.20
High myopia in adulthood often begins as “school-age myopia”; therefore, intervention in these early stages to reduce myopia onset and/or progression will have lifelong impacts with significant socioeconomic benefits.
Appropriate early referral for optometric assessment and prescription of glasses or contact lenses is encouraged, as under-correction of myopia is associated with increased progression and higher myopic outcomes.21
In addition, there are numerous options for myopia control treatments, which aim to reduce the axial elongation of the eye and subsequent increasing myopia. Effective options available include specialist spectacle lenses, overnight hard contact lenses that temporarily reshape the cornea (orthokeratology), and antimuscarinic topical ocular medication, such as atropine.21
More information on simple environmental changes to influence myopia development and progression, such as increased outdoor time, can be found at: outdoorplay.nz
Change in refraction with age is expected and is part of normal growth and emmetropisaton (the minimisation of refractive error) of the eye
All children born in New Zealand should have an eye check as part of their neonatal assessment, with details outlined in the Well Child / Tamariki Ora Programme Practitioner Handbook. 22
In children where visual behaviour or development is abnormal, or in the presence of nystagmus, referral for a comprehensive eye examination is required.
The GP has a vital role to play in identifying mild to severe reduced vision in children. The following tests should be considered when examining a child with a vision concern:
- Perform a red reflex test to check ocular media clarity (details below).
- Measure unaided visual acuity binocularly and monocularly, when possible (details below). When applicable, also measure with habitual correction or a pinhole – a pinhole measurement will improve visual acuity for refractive causes of reduced unaided vision but not for other causes.
- Check ocular motility with an interesting toy or a red target.
- Check the anterior aspect of the eye for gross abnormalities such as conjunctival injection, corneal opacification or an obvious cataract. An ophthalmoscope used from ~10cm with a +10DS lens “dialled in” can give you a magnified view of the anterior segment.
- Check the optic nerve and macula for abnormalities such as optic nerve pallor or swelling, macula pigmentation or damage. This can be completed with an ophthalmoscope with lenses set to zero if the practitioner has no refractive error or is wearing their corrective lenses (glasses or contact lenses).
Red reflex test
The red reflex test is a simple, non invasive screening technique:23
- A normal red reflex, as defined by the American Academy of Pediatrics, is equal in colour and intensity, and symmetric in both eyes, with no dark spots, opacities or white reflexes (Figure 5).
- An abnormal red reflex can indicate sight-threatening, life-threatening or systemically associated conditions, such as congenital cataracts, retinoblastoma or metabolic disorders.
In New Zealand, all infants with an abnormal red reflex or a family history of inherited ocular disorders should be referred for a comprehensive ophthalmic examination.22,23
The sensitivity of the red reflex test is limited as it is a screening tool – when compared with a comprehensive eye examination, a sensitivity of 99.6 per cent for anterior segment disease (cornea, iris and lens) but only 4.1 per cent for posterior segment disease (structures behind the lens) was reported.24 However, in practice, case detection is probably lower than these reported figures.
In the UK, where red reflex screening is standard practice, a retrospective review of congenital cataract detection indicated that by eight weeks of age, only 47 per cent of cases had been identified.25
For posterior segment disease detection, a study of dilated red reflex examination of 37 paediatric eyes by a paediatric ophthalmologist failed to detect any of the 13 cases of retinoblastoma in an at-risk group.26
Reasons for the reduced detection rates are likely multifactorial and, in all likelihood, related to inadequate training,27 incorrect implementation of the red reflex test,28 as well as the sensitivity of the test itself.24
Therefore, without overcoming logistical, test sensitivity and educational challenges, vision-impairing ocular opacities and posterior segment disease may still be missed.25
However, the red reflex test remains a very useful screening tool when performed appropriately.
The red reflex test can also be useful for older children and even adults to check the clarity of the ocular media, but this should be used in conjunction with visual acuity measurements, observance of visual behaviour, and gross ocular assessment with an ophthalmoscope.
Visual acuity measurement
Visual acuity is the key measure of clarity of vision. Visual acuity starts at approximately 0.15 logMAR (6/180) at one month of age and develops to adult-equivalent vision of 0.0 logMAR (6/6) by five years.29,30
Methods for assessing this varying vision must be age and developmental stage appropriate:
- Preferential looking techniques, such as Cardiff or Teller cards, are appropriate for preverbal or cognitively impaired children.29,31
- The LEA Symbols Test is appropriate for preschool children, with a success rate of 76 per cent at age three and 95 per cent at age four, as well as high comparability to the Landolt C.32
- Compliance with quantitative letter-based acuity testing can be achieved in the majority of cognitively normal five-year-olds.31
- The ETDRS chart (developed for the Early Treatment Diabetic Retinopathy Study) has high repeatability measures in school-aged children with refractive errors.33
In all measures of visual acuity with a chart, ensure it is well lit, the child is at the appropriate distance away and the chart has maintained its contrast. Record the visual acuity, eye used, whether aided or unaided, distance of measurement and type of chart used.
In general practice, it is not common to have a large range of visual acuity tests available; therefore, using the tools you have available in the appropriate manner, and referring when further information is required, is recommended. Continually praising children encourages them to maintain focus and attempt smaller optotypes during threshold visual acuity testing.
When only a letter chart is available for a young child, you can consider using a matching card – a printed card with the letters on it – for the child to match to rather than needing to name the letters. These can be particularly helpful with shy children.
In even younger children, assessment of fixing and following at a set, recorded distance is appropriate. A small, colourful toy is an excellent tool to use for this.
In addition, a simple “objection to occlusion” test can be used. The child’s eyes are covered in turn with the palm of your hand, and equal objection to occluding them is a “normal” result. The amount of protest is often child dependent, so comparison of protest is the measure.
For example, a child with severely reduced vision in the right eye will not protest much when the right eye is covered; however, if the left eye is covered, they will protest as you have covered up their main view of the world. This difference in response is recorded as “unequal objection to occlusion” and indicates a possible difference in vision between the eyes, requiring referral for further assessment.
When referring cases and reduced vision is suspected, a visual acuity measurement is beneficial – ideally both binocular and monocular results. If not possible, then simply stating “concern of reduced visual acuity in both/right/left eye(s)” is suitable.
In a clinical setting, it is important to have a low threshold for referral of paediatric ocular conditions for further detailed examination.
B4 School Vision Screening
Reduced visual acuity and uncorrected refractive error (myopia, hyperopia or astigmatism) impact on academic performance, including reduced early literacy scores.34
B4 School Vision Screening is undertaken by vision and hearing technicians between a child’s fourth and fifth birthdays. Increased accuracy of screening has been reported with increasing age, and this may be due to the visual acuity letter test.
The screening is designed to detect amblyopia; however, due to the nature of the screening test, it also detects reduced distance vision from other causes. Hyperopia (long-sightedness) and strabismus (eye turns) are often not detected through this screening test.18
If bilateral reduced vision or a significant difference between the eyes is detected, then referral for optometric or ophthalmic examination is warranted, with exact referral guidelines varying between DHBs.
B4 School Vision Screening is important to diagnose and treat children with reduced distance visual acuity, but will not capture all children requiring refractive correction. In the case of myopia, most children who go on to develop myopia will not have developed it in time to be detected at this early screening.
Change in refraction with age is expected and is part of normal growth and emmetropisation (the minimisation of refractive error) of the eye. Infants are born hyperopic with an average axial length less than 17mm. The majority of ocular growth occurs before 24 months, and the emmetropisation process is completed between six and eight years of age.35 However, refractive error can continue to change throughout childhood for some children, leading to myopia.
Key support services
Vision is a key sense for function, development and education. From birth, vision develops throughout childhood. Therefore, it is important to detect anything impacting on this development and to either treat or support children with visual impairment. In addition to local optometric and ophthalmic services, there are specific support services for children with visual impairment.
Blind Low Vision NZ (blindlowvision.org.nz) is the national charity supporting all New Zealanders, not just children, who are blind or have low vision. Blind Low Vision NZ provides counselling services, orientation and mobility, and has an amazing library of alternative access books. Referral criteria for Blind Low Vision NZ are a visual acuity of 6/24 or worse in the better eye, or significantly reduced peripheral vision. There is no age restriction.
Blind Low Vision NZ has a specialist team to provide cultural support to Pacific clients, while Kāpō Māori Aotearoa provides cultural services for Māori clients. Kāpō Māori Aotearoa (kapomaori.com) is a national kaupapa Māori provider of peer support and health and disability services. It is a member-based society open to all people (disabled, able-bodied, Māori and non-Māori) and has an established reputation in the blindness community.
The key service for children is the Blind and Low Vision Education Network NZ (BLENNZ; blennz.school.nz), which is part of the Ministry of Education. BLENNZ is a school made up of a national network of educational services for ākonga (learners) who are blind, deafblind or have low vision. It provides a range of services, including teaching support in schools, orientation and mobility, low vision aids, specific immersion courses, and a specialist transdisciplinary national assessment when required.
BLENNZ supports children and young people with low vision and blindness to achieve their potential in education. Referral criteria for BLENNZ are a visual acuity of 6/18 or worse in the better eye, significantly reduced peripheral vision, or cerebral visual impairment affecting curriculum access.
The Ministry of Education has funding via the Ongoing Resourcing Scheme specifically for children with reduced vision. BLENNZ organises ORS applications and support for these children.
Other support groups available include Parents of Vision Impaired (pvi.org.nz). PVI is made up of parents of children who are blind or visually impaired, who aim to support other parents in the same position. They provide shared experience, support and advocacy from their unique experience and perspective.
The GP can also provide referral for treatment and refractive correction. A relationship with the local optometrist and ophthalmologist with paediatric interests can be a fantastic resource in managing this patient population.
Samantha Simkin is a research fellow and optometrist for Blind and Low Vision Education Network NZ, and works as an optometrist in private practice. Dr Simkin is a therapeutically qualified optometrist with a PhD in childhood visual impairment. She continued her research as the Stevenson postdoctoral research fellow at the University of Auckland.
Mo Ziaei is a cornea and anterior segment specialist at Re:Vision Laser and Cataract, and at Greenlane Clinical Centre. He is also a senior lecturer at the University of Auckland.
This 10-question assessment is designed to demonstrate that the provided educational reading has been effective in allowing you to meet the learning objectives of this course. Write down your answers to these questions.
1. What is the critical period for vision development?
a. Birth to age three or four years
b. Birth to age seven or eight years
c. Birth to puberty
d. Birth to adulthood
2. In children with congenital cataracts, timely surgical intervention is essential. When does this typically this occur?
a. Before six weeks of age for all cases
b. Between six and eight weeks of age for all cases
c. Between six and eight weeks of age for bilateral cases, and before six weeks for unilateral cases
d. Between six and eight weeks of age for unilateral cases, and before six weeks for bilateral cases
3. Which of the following causes of paediatric visual impairment is often described by parents as a “golden glow” in the pupil?
a. Albinism
b. Congenital cataract
c. Retinoblastoma
d. Optic nerve hypoplasia
4. Which of the following is caused by (often preventable) central nervous system damage to the visual system posterior to the chiasm?
a. Amblyopia
b. Cerebral visual impairment
c. Myopia
d. Optic nerve hypoplasia
5. Which of the following best describes the appearance of optic nerve hypoplasia upon examination with an ophthalmoscope?
a. A small optic disc, often inside a ring of hypopigmentation
b. An elevated optic disc with blurred margins
c. Iris transillumination defects
d. Prominent temporal pallor of the optic disc
6. Which THREE of the following can cause amblyopia?
a. Refractive errors, such as myopia
b. Strabismus
c. Structural abnormalities of the eye
d. Visual deprivation, such as cataracts
7. Which TWO statements regarding the examination of a child with a vision concern are correct?
a. A pinhole measurement will improve visual acuity for refractive causes of reduced unaided vision but not for other causes
b. Examination of the anterior segment of the eye is performed with the ophthalmoscope lens set to zero
c. Ocular motility should be checked with an interesting toy or a red target
d. The red reflex test is no longer recommended as a screening tool due to sensitivity limitations
8. Which visual acuity test would be most suitable for a child aged three to four years.
a. A Snellen or logMAR chart
b. Preferential looking techniques
c. The ETDRS chart
d. The LEA Symbols Test
9. When performing the objection to occlusion test, how would a child with significantly reduced vision in the left eye typically respond?
a. They protest equally to each eye being covered, but more so than a child with unaffected vision
b. They protest more when the left eye is covered than the right eye
c. They protest more when the right eye is covered than the left eye
10. What are the criteria for referring a child to Blind Low Vision NZ?
a. Any child with a documented eye condition that reduces their vision and impacts their learning
b. Only adults can be referred; children should be referred to Blind and Low Vision Education Network NZ instead
c. Visual acuity of 6/24 or worse in the better eye, or significantly reduced peripheral vision
d. Visual acuity of 6/18 or worse in the better eye, or significantly reduced peripheral vision
Write down your answers to these questions. Then, to check your answers and record your score, click here.
You can use the Capture button below to record your time spent reading and your answers to the following learning reflection questions:
- Why did you choose this activity (how does it relate to your professional development plan learning goals)?
- What did you learn?
- How will you implement the new learning into your daily practice?
- Does this learning lead to any further activities that you could undertake (audit activities, peer discussions, etc)?
We're publishing this Educate article as a FREE READ so it is FREE to read and EASY to share more widely. If you would like to access news and comprehensive primary care education, and support us – subscribe here
1. You C, Wu X, Zhang Y, et al. Visual impairment and delay in presentation for surgery in Chinese pediatric patients with cataract. Ophthalmology 2011;118(1):17–23.
2. Ram J, Gupta N, Sukhija JS, et al. Outcome of cataract surgery with primary intraocular lens implantation in children. Br J Ophthalmol 2011;95(8):1086–90.
3. Gilbert C, Foster A. Childhood blindness in the context of VISION 2020: The right to sight. Bull World Health Organ 2001;79(3):227–32.
4. Magnusson G, Bizjajeva S, Haargaard B, et al. Congenital cataract screening in maternity wards is effective: Evaluation of the paediatric cataract register of sweden. Acta paediatrica 2013;102(3):263–67.
5. Zetterström C, Kugelberg M. Paediatric cataract surgery. Acta Ophthalmol Scand 2007;85(7):698–710.
6. Lesueur LC, Arné JL, Chapotot EC, et al. Visual outcome after paediatric cataract surgery: Is age a major factor? Br J Ophthalmol 1998;82(9):1022–25.
7. Birch EE, Cheng C, Stager DR, et al. The critical period for surgical treatment of dense congenital bilateral cataracts. J AAPOS 2009;13(1):67–71.
8. Birch EE, Stager DR. The critical period for surgical treatment of dense congenital unilateral cataract. Invest Ophthalmol Vis Sci 1996;37(8):1532–38.
9. Kivela T. The epidemiological challenge of the most frequent eye cancer: Retinoblastoma, an issue of birth and death. Br J Ophthalmol 2009;93(9):1129–31.
10. MacCarthy A, Birch JM, Draper GJ, et al. Retinoblastoma: Treatment and survival in great britain 1963 to 2002. Br J Ophthalmol 2009;93(1):38–39.
11. Kong L, Fry M, Al-Samarraie M, et al. An update on progress and the changing epidemiology of causes of childhood blindness worldwide. J AAPOS 2012;16(6):501–07.
12. Chong C, Dai S. Cross-sectional study on childhood cerebral visual impairment in New Zealand. J AAPOS 2014;18(1):71–74.
13. Goh YW, Andrew D, McGhee C, et al. Clinical and demographic associations with optic nerve hypoplasia in New Zealand. Br J Ophthalmol 2014;98(10):1364–67.
14. Garcia-Filion P, Epport K, Nelson M, et al. Neuroradiographic, endocrinologic, and ophthalmic correlates of adverse developmental outcomes in children with optic nerve hypoplasia: A prospective study. Pediatrics 2008;121(3):653.
15. Gronskov K, Ek J, Brondum-Nielsen K. Orphanet journal of rare diseases. Orphanet Journal of Rare Diseases 2007;2:43.
16. Kirkwood B. Albinism and its implications with vision. Insight 2009;34(2):13–16.
17. Wilson GA, Welch D. Does amblyopia have a functional impact? findings from the Dunedin multidisciplinary health and development study. Clin Experiment Ophthalmol 2013;41(2):127–34.
18. Hamm LM, Findlay R, Black JM. 7 Vision screening in infancy and childhood. In: Cutfield WS, Derraik JGB, Waetford C, et al (Eds). Brief Evidence Reviews for the Well Child Tamariki Ora Programme, pp. 168–216. Auckland, NZ: A Better Start National Science Challenge; 2019.
19. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016;123(5):1036–42.
20. Wong TY, Ferreira A, Hughes R, et al. Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: An evidence-based systematic review. Am J Ophthalmol 2014;157(1):9–25.e12.
21. Walline JJ, Lindsley KB, Vedula SS, et al. Interventions to slow progression of myopia in children. Cochrane Database Syst Rev 2020;1(1):CD004916.
22. Ministry of Health. Well Child / Tamariki Ora Programme Practitioner Handbook: Supporting families and whānau to promote their child’s health and development. Wellington, NZ: Ministry of Health; 2014.
23. American Academy of Pediatrics, Section on Ophthalmology; American Association for Pediatric Ophthalmology And Strabismus; American Academy of Ophthalmology; American Association of Certified Orthoptists. Red reflex examination in neonates, infants, and children. Pediatrics 2008;122(6):1401–04.
24. Sun M, Ma A, Li F, et al. Sensitivity and specificity of red reflex test in newborn eye screening. J Pediatr 2016;179:192–96.e4.
25. Rahi JS, Dezateux C. National cross sectional study of detection of congenital and infantile cataract in the united kingdom: Role of childhood screening and surveillance. BMJ 1999;318(7180):362–65.
26. Khan AO, Al-Mesfer S. Lack of efficacy of dilated screening for retinoblastoma. J Pediatr Ophthalmol Strabismus 2005;42(4):205–10.
27. Raoof N, Dai S. Red reflex screening in New Zealand: A large survey of practices and attitudes in the Auckland region. N Z Med J 2016;129(1438):38–43.
28. Fry M, Wilson GA. Scope for improving congenital cataract blindness prevention by screening of infants (red reflex screening) in a New Zealand setting. J Paediatr Child Health 2005;41(7):344–46.
29. Mayer DL, Beiser AS, Warner AF, et al. Monocular acuity norms for the teller acuity cards between ages one month and four years. Invest Ophthalmol Vis Sci 1995;36(3):671–85.
30. Salomao SR, Ventura DF. Large sample population age norms for visual acuities obtained with vistech-teller acuity cards. Invest Ophthalmol Visual Sci 1995;36(3):657–70.
31. Solebo AL, Rahi J. Epidemiology, aetiology and management of visual impairment in children. Arch Dis Child 2014;99(4):375–79.
32. Becker R, Hubsch S, Graf MH, et al. Examination of young children with lea symbols. Br J Ophthalmol 2002;86(5):513–16.
33. Manny RE, Hussein M, Gwiazda J, et al. Repeatability of ETDRS visual acuity in children. Invest Ophthalmol Vis Sci 2003;44(8):3294–300.
34. Hopkins S, Narayanasamy S, Vincent SJ, et al. Do reduced visual acuity and refractive error affect classroom performance? Clinical and Experimental Optometry 2020;103(3):278–89.
35. West CE. Refractive error in children. In: Wilson ME, et al (Eds). Pediatric Ophthalmology, pp 7–20. Springer; 2009.










![Barbara Fountain, editor of New Zealand Doctor Rata Aotearoa, and Paul Hutchison, GP and senior medical clinician at Tāmaki Health [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/Barbara%20Fountain%2C%20editor%20of%20New%20Zealand%20Doctor%20Rata%20Aotearoa%2C%20and%20Paul%20Hutchison%2C%20GP%20and%20senior%20medical%20clinician%20at%20T%C4%81maki%20Health%20CR%20Simon%20Maude.jpg?itok=-HbQ1EYA)
![Lori Peters, NP and advanced health improvement practitioner at Mahitahi Hauora, and Jasper Nacilla, NP at The Terrace Medical Centre in Wellington [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/2.%20Lori%20Peters%2C%20NP%20and%20advanced%20HIP%20at%20Mahitahi%20Hauora%2C%20and%20Jasper%20Nacilla%2C%20NP%20at%20The%20Terrace%20Medical%20Centre%20in%20Wellington%20CR%20Simon%20Maude.jpg?itok=sUfbsSF1)
![Ministry of Social Development health and disability coordinator Liz Williams, regional health advisors Mary Mojel and Larah Takarangi, and health and disability coordinators Rebecca Staunton and Myint Than Htut [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/3.%20Ministry%20of%20Social%20Development%27s%20Liz%20Williams%2C%20Mary%20Mojel%2C%20Larah%20Takarangi%2C%20Rebecca%20Staunton%20and%20Myint%20Than%20Htut%20CR%20Simon%20Maude.jpg?itok=9ceOujzC)
![Locum GP Helen Fisher, with Te Kuiti Medical Centre NP Bridget Woodney [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/4.%20Locum%20GP%20Helen%20Fisher%2C%20with%20Te%20Kuiti%20Medical%20Centre%20NP%20Bridget%20Woodney%20CR%20Simon%20Maude.jpg?itok=TJeODetm)
![Ruby Faulkner, GPEP2, with David Small, GPEP3 from The Doctors Greenmeadows in Napier [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/5.%20Ruby%20Faulkner%2C%20GPEP2%2C%20with%20David%20Small%2C%20GPEP3%20from%20The%20Doctors%20Greenmeadows%20in%20Napier%20CR%20Simon%20Maude.jpg?itok=B0u4wsIs)
![Rochelle Langton and Libby Thomas, marketing advisors at the Medical Protection Society [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/6.%20Rochelle%20Langton%20and%20Libby%20Thomas%2C%20marketing%20advisors%20at%20the%20Medical%20Protection%20Society%20CR%20Simon%20Maude.jpg?itok=r52_Cf74)
![Specialist GP Lucy Gibberd, medical advisor at MPS, and Zara Bolam, urgent-care specialist at The Nest Health Centre in Inglewood [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/7.%20Specialist%20GP%20Lucy%20Gibberd%2C%20medical%20advisor%20at%20MPS%2C%20and%20Zara%20Bolam%2C%20urgent-care%20specialist%20at%20The%20Nest%20Health%20Centre%20in%20Inglewood%20CR%20Simon%20Maude.jpg?itok=z8eVoBU3)
![Olivia Blackmore and Trudee Sharp, NPs at Gore Health Centre, and Gaylene Hastie, NP at Queenstown Medical Centre [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/8.%20Olivia%20Blackmore%20and%20Trudee%20Sharp%2C%20NPs%20at%20Gore%20Health%20Centre%2C%20and%20Gaylene%20Hastie%2C%20NP%20at%20Queenstown%20Medical%20Centre%20CR%20Simon%20Maude.jpg?itok=Z6u9d0XH)
![Mary Toloa, specialist GP at Porirua and Union Community Health Service in Wellington, Mara Coler, clinical pharmacist at Tū Ora Compass Health, and Bhavna Mistry, specialist GP at Porirua and Union Community Health Service [Image: Simon Maude]](/sites/default/files/styles/thumbnail_cropped_100/public/2025-03/9.%20Mary%20Toloa%2C%20Porirua%20and%20Union%20Community%20Health%20Service%20in%20Wellington%2C%20Mara%20Coler%2C%20T%C5%AB%20Ora%20Compass%20Health%2C%20and%20Bhavna%20Mistry%2C%20PUCHS%20CR%20Simon%20Maude.jpg?itok=kpChr0cc)