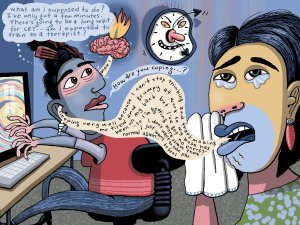
A range of approaches is needed to manage mental health presentations. In this article, specialist GP Sophie Jadwiga Ball describes two tools that can be employed within a GP consultation and provides the evidence-based theory behind their use. She also presents numerous examples to demonstrate how you can apply these tools in practice
A medical alarm can support the independence of your older patients
A medical alarm can support the independence of your older patients

Family members and healthcare workers also gain peace of mind in knowing that their older relatives and patients can access help by simply pressing an alarm button.10
The independence of older adults is facilitated by living in their own homes as it enables greater autonomy and closer connections with their family, friends, and community. Living at home for as long as possible is highly valued by older adults,1 and is consistent with social policy that older adults should ‘age in place’ including those who require care and support.2
Studies suggest that maintaining independence is the most important health outcome for older patients when faced with a treatment decision.3,4 Living independently requires people to undertake activities of daily living, which is associated with functional independence and improved quality of life.5
Older adults are at high risk of a complicated recovery post-hospital discharge, including functional losses, adverse medical events such as falls, and rehospitalisation.6,7 Hence, seniors may require increased care needs at home, and highlights the need for appropriate planning for care post-discharge.
Restorative and intermediate care plans to support ageing in place have been demonstrated to be effective in improving the health-related quality of life of older adults and in facilitating their transition from medical dependence to functional independence.8,9 These types of plans allow older adults to remain living at home as a viable alternative to age-related residential care,8 and is consistent with their desire to live for as long as possible in their own home.1
Encouraging ageing in place is likely to increase demand for community care services.10,11 To ease some of this pressure, technological innovations, such as a personal medical alarm have been promoted as an approach to lessen pressure on home care services.
A medical alarm can complement planned care by facilitating rapid medical response when activated by a patient.12 It can also give users the confidence to maintain an active life,10 which is consistent with the focus of healthcare in older adults being able to maintain their functional capabilities.13
Family members and healthcare workers also gain peace of mind in knowing that their older relatives and patients can access help by simply pressing an alarm button.10
Community-dwelling older adults who are the typical users of a personal medical alarm, are likely to consider a device if the suggestion comes from a healthcare professional.11
Referring a St John Medical Alarm as part of the home care plan for your older patients provides them with 24/7 access to expert care and is the only direct link to Hato Hone St John, instilling the confidence to live a more independent life.
The referral process is straightforward using your Practice Management System via Healthlink or ERMS and your patients have access to a FREE trial.
For additional information visit: stjohnalarms.org.nz/hcp
1. van Leeuwen KM, et al. What does quality of life mean to older adults? A thematic synthesis. PLoS One. 2019;14(3):e0213263.
2. Davey J. "Ageing in Place": The views of older homeowners on maintenance, renovation and adaptation. Soc Policy J N Z. 2006(27):128-41.
3. Festen S, et al. 'What matters to you?' Health outcome prioritisation in treatment decision-making for older patients. Age Ageing. 2021;50(6):2264-9.
4. Fried TR, et al. Health outcome prioritization as a tool for decision making among older persons with multiple chronic conditions. Arch Intern Med. 2011;171(20):1854-6.
5. Mlinac ME, et al. Assessment of Activities of Daily Living, Self-Care, and Independence. Arch Clin Neuropsychol. 2016;31(6):506-16.
6. Dodson, John A, et al. Physical function and independence one year following myocardial infarction: observations from the TRIUMPH registry. Am Heart J. 2012;163(5):790-6.
7. Resnick, B, et al. Optimizing physical activity among older adults post trauma: overcoming system and patient challenges. Int J Orthop Trauma Nurs. 2015;19(4):94-206.
8. Parsons M, et al. The Assessment of Services Promoting Independence and Recovery in Elders Trial (ASPIRE): a pre-planned meta-analysis of three independent randomised controlled trial evaluations of ageing in place initiatives in New Zealand. Age Ageing. 2012;41(6):722-8.
9. King A, et al. Assessing the impact of a restorative home care service in New Zealand: a cluster randomised controlled trial. Health Soc Care Community. 2012;20(4):365-74.
10. Stokke R. "Maybe we should talk about it anyway": a qualitative study of understanding expectations and use of an established technology innovation in caring practices. BMC Health Serv Res. 2017;17(1):657.
11. Stokke R. The Personal Emergency Response System as a Technology Innovation in Primary Health Care Services: An Integrative Review. J Med Internet Res. 2016;18(7):e187.
12. Agboola S, et al. Healthcare utilization in older patients using personal emergency response systems: an analysis of electronic health records and medical alert data : Brief Description: A Longitudinal Retrospective Analyses of healthcare utilization rates in older patients using Personal Emergency Response Systems from 2011 to 2015. BMC Health Serv Res. 2017;17(1):282.
13. Beck P. Chapter 225. In: Walker HK, et al., editors. Clinical Methods: The History, Physical, and Laboratory Examinations 3rd Edition. The Elderly Patient. Vol. Boston: Butterworth Publishers, a division of Reed Publishing. 1990.