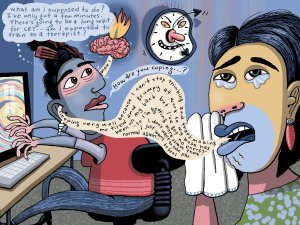
A range of approaches is needed to manage mental health presentations. In this article, specialist GP Sophie Jadwiga Ball describes two tools that can be employed within a GP consultation and provides the evidence-based theory behind their use. She also presents numerous examples to demonstrate how you can apply these tools in practice
The importance of timely treatment for CVD events
The importance of timely treatment for CVD events

It is already well-understood that timely intervention is essential to mitigate the effects of cardiovascular events. That is particularly relevant when it comes to adults aged over 65 years, for whom the prevalence of heart attack, stroke and heart failure is highest.1
Assessment of your older patients regarding their vulnerability to cardiovascular disease (CVD) should ideally include consideration of their home environment. If they live independently or are likely to be on their own for extended periods, then it might be appropriate to consider recommending a personal emergency response device such as a medical alarm when tailoring their care plan.
The key to acute management of heart attacks is the amount of time it takes to restore the coronary artery blood flow.2,3 The sooner that percutaneous coronary intervention (PCI) can be performed (typically within 12 hours of coronary occlusion), the better the chance of a good outcome. Total time to performance of PCI is the sum of onset-to-door time (OTD: time between symptom onset and hospital arrival) and door-to-balloon time (DTB: time between hospital arrival and performance of PCI).
Compared with longer DTB (≥90 mins) and OTD (≥4 hrs) times, patients with acute heart attack requiring PCI who had shorter DTB (<90 mins) and OTD (<4 hrs) times had lower longer-term mortality (3.51% vs 7.25%).4 Demonstrating the strong effect of travel time on clinical outcome, a longer OTD time (≥4 vs <4 hrs) was associated with significantly (p<0.03) higher longer-term mortality despite a shorter DTB time (<90 vs >90 mins).4
The need for early treatment is even more critical for stroke patients, with thrombolytic therapy having a therapeutic window of only several hours.5,6 Initiating therapy within this narrow window is essential for improved outcomes. Stroke patients who used an ambulance were more likely to reach the hospital and be treated with thrombolytic therapy within the therapeutic window than non-ambulance users (64.6% vs 29.6%; p<0.001).5 The OTD time was significantly shorter for ambulance users than for non-ambulance users (32 vs 44.5 min; p<0.001).
Patients whose health status is diminished following either a heart attack, stroke, or the onset of heart failure risk loss of functionality,8 and their ability to continue to live independently may be threatened.
Delayed treatment, for whatever reason, in patients experiencing exacerbation of their heart failure symptoms has been demonstrated to be significantly associated with an increased risk of rehospitalisation and mortality after discharge.7
Patients whose health status is diminished following either a heart attack, stroke, or the onset of heart failure risk loss of functionality,8 and their ability to continue to live independently may be threatened. Acute and chronic post stroke health status are especially undesirable, with the functional impact likely to involve cognitive and mobility impairments. The acute health state after a heart attack is also associated with reduced function. At least four in every ten survivors of a heart attack requiring hospitalisation experience clinically relevant declines in physical functioning in the year following the event.9
Intervention strategies are recommended to reduce the pre-hospital delay so that medical care for CVD events is received within the therapeutic window, thereby likely improving clinical outcomes and the ability to live independently. A personal emergency response such as a medical alarm can be an appropriate solution to this need.
Referring a St John Medical Alarm can offer your older patients 24/7 response and is the only alarm that links directly to Hato Hone St John. As part of the treatment plan for your older patients, access to help through a medical alarm can instil the confidence to live a more independent life.
Referral is straightforward through your Practice Management System via Healthlink or ERMS and your patients have access to a free trial.
For additional information go to stjohnalarms.org.nz/hcp
1. Ministry of Health 2023: NZ Health Survey Annual Data Explorer (July 2021 to July 2022). 2. Dauerman HL, et al. J Am Coll Cardiol. 2021;77(15):1871-4. 3. Ojha N and Dhamoon NO. StatPearls Publishing 2022: Myocardial Infarction. 4. Hannan EL, et al. Am J Cardiol. 2010;106(2):143-7. 5. Lau KK, et al. Hong Kong Med J. 2018;24(4):335-9. 6. Sozener CB, et al. Ann N Y Acad Sci. 2012;1268:51-6. 7. Lin CY, et al. Eur J Cardiovasc Nurs. 2021;20(5):454-63. 8. Matza LS, et al. BMC Health Serv Res. 2015;15:173. 9. Dodson JA, et al. Am Heart J. 2012;163(5):790-6.